Author(s): Robert J Diecidue, Brandon M Locke and Joseph D Harrington*
Head and neck cancers pose a significant challenge to clinicians to treat the disease while limiting the amount of morbidity to the patient. Given this need, new trials and medications have been explored to provide tissue sparing therapies. One of these methods being trialed at our institution is photoimmunotherapy with the PD1 inhibitor pembrolizumab. A patient with multiple recurrences of squamous cell carcinoma of the oral cavity underwent trial with photoimmunotherapy, but developed severe lip ulceration and swelling that required the patient to discontinue the trial. Biopsy and antibody testing revealed elevated levels of BP180 and BP230 indicating bullous pemphigoid. In addition, elevated Envoplakin was noted confirming a simultaneous paraneoplastic pemphigus diagnosis. Given the growing number of case reports showing an association of paraneoplastic pemphigus and bullous pemphigoid with pembrolizumab and other PD1 inhibitors, further investigation should be undertaken to better understand the incidence of these diseases with photoimmunotherapy.
Head and neck cancer is a challenging disease to treat, and has a significant associated morbidity and mortality. Worldwide these cancers account for both 5.3% of all cancers, and all cancer deaths. Over the last 20 years the rates of oral cavity cancers have risen [1]. To date the main modality of treatment remains surgical resection of the cancerous lesions [2]. Advances in diagnostics and adjuvant treatment have led to increases in the five-year survival rates of these patients [3]. For tumors that have advanced TNM staging or adverse features, adjuvant treatments such as radiation therapy and chemotherapy have been employed [4]. However,despite these advances, unfortunately surveillance for local and distant recurrence remains a feature of these patients’ treatment course. These cases can be challenging, as reducing further morbidity from tissue loss must be accounted for. Innovation has led to the introduction of photodynamic therapy and immunotherapy as possible tissue sparing treatment methods, especially in recurrent cases and prior radiation [5,6]. Photodynamic therapy generates reactive oxygen species which causes damage to the cancer cells by causing direct phototoxicity, compromising tumor vasculature, and inducing inflammatory reactions that enable systemic immunity [7,8]. Currently at our institution, there are ongoing trials using photoimmunotherapy as adjuncts for advanced stage tumors and recurrent cases. The goal of this trialed therapy is more selective tumor cell targeting with the hopes of also mitigating adverse effects on surrounding cells [9]. This is accomplished through combining the action of reactive oxygen species produced by photodynamic therapy paired with the high specificity of antibody targeting when T-cell action is reactivated through PD1 inhibition [10,11].
As with all developing treatments undergoing active trials, there are unknown potential adverse effects. In addition to bullous pemphigoid that can at times noted following immunotherapy, one such rare emerging complication is paraneoplastic pemphigus which is a form of the autoimmune mucocutaneous disease that is associated with patients who have underlying neoplasm [12]. This disease is most commonly seen in patients who have hematologic malignancies which account for 84% of reported cases of the disease, while only approximately 8% can be attributed to epithelial origin carcinomas [13]. There have been several case reports demonstrating an association between the use of pembrolizumab, a PD1 inhibitor, and the incidence of bullous pemphigoid as well as paraneoplastic pemphigus. In these cases, either a primary eruption or subclinical case that flared were found with initiation of the immunotherapy. Interestingly, these were in cases on non-hematologic malignancies [14,15]. We present a case, where a patient with oral squamous cell carcinoma was initiated on pembrolizumab and photodynamic therapy and developed a severe adverse reaction which was ultimately found to be a case of simultaneous bullous pemphigoid and paraneoplastic pemphigus. Due to the timeliness of the disease manifestation following the trialed treatment, it leads to difficulty in attributing the paraneoplastic pemphigus to solely the pembrolizumab or the combined photoimmunotherapy.
We present a case of a complication associated with a patient’s treatment with photoimmunotherapy for recurrent squamous cell carcinoma of the oral cavity. At the time of her initial presentation in June of 2018, the patient was a 54-year-old female with a past medical history significant for hypertension, and lichen planus that was confirmed by biopsy by her dentist in 2014. Additionally, she had social history significant for a 15 pack- year smoking history. Ultimately, she noticed a growing mass of her right tongue/floor of mouth and in June of 2018 she had a biopsy of the right floor of mouth and was diagnosed with papillary squamous cell carcinoma, which was noted to be well differentiated on histopathology. She subsequently underwent a right partial glossectomy, floor of mouth resection, ipsilateral neck dissection of levels I-IV, and reconstruction with a radial forearm free flap. Final surgical pathology from her initial tumor was a pT3N0, resected to negative margins, 0/49 lymph nodes positive for tumor, positive lymph vascular invasion, and depth of invasion of 4 mm. She was recommended to undergo adjuvant radiation therapy, which she began within 6 weeks of her surgery and received a total of 6000 cGy.
Following her initial treatment, she unfortunately developed a recurrence in November of 2019. She was found to have a leukoplakia of her right retromolar trigone and tongue which was biopsied and showed severe dysplasia. She was again taken to the OR in December of 2019 for resection of the right RMT and partial glossectomy. The lesion was found on final pathology to be a squamous cell carcinoma rpT1Nx with a DOI of 3 mm excised to negative margins. She was continued on observation at that time. Shortly after this procedure in March of 2020 she developed a new area of concern along the left floor of mouth that was biopsied and found to be another recurrence of squamous cell carcinoma. In the same month she was then taken again to the OR for a wide local excision of the left floor of mouth, partial glossectomy, and marginal mandibulectomy. This tumor was also found to be a rpT1Nx with a DOI of 2 mm, tumor extending to the anterior margin, with a focus of perineural invasion. She was again discussed at the tumor board at our institution and, given the small size of the primary lesion and history of radiation, she was continued on observation.
In October of 2020, she presented to our practice due to concern for radiation caries of tooth #18. This was confirmed on physical examination and radiographic evaluation. Due to the patient’s history of radiation, she was sent for Hyperbaric Oxygen Therapy based upon the Marx Protocol of 20 dives prior to extractions and 10 post-operatively [16,17]. She underwent extraction, and her wound healed uneventfully.
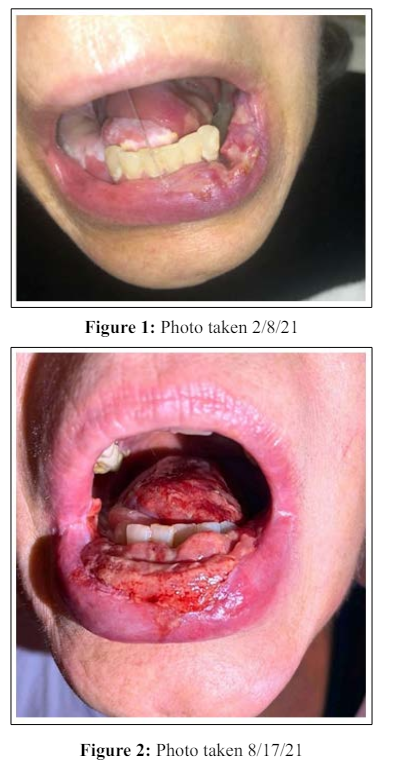
During observation she developed a new lesion of her left lateral tongue, which was biopsied and found to be consistent with a rcT2N0 squamous cell carcinoma. At this point, due to this being her third recurrence, clinical trials were discussed and she was ultimately enrolled in a photoimmunotherapy trial. As part of this trial, she would receive treatment with pembrolizumab and light therapy. She began the trial on January 15, 2021 where she received pembrolizumab 200 mg, and then underwent photodynamic therapy on January 21, 2021. Within one-week post-op, she began to develop a left sided lip inflammatory lesion, initially treated with magic mouthwash, which is typically used to treat oral sores and lesions caused by cancer therapies. She received her second infusion of pembrolizumab on February 4, 2021. She continued to have worsening pain, ulceration, and swelling of her lips and was started on a Medrol dose pack prior to her third pembrolizumab infusion on February 26, 2021.
At this point the patient had developed a severe reaction, and had significant lip swelling and ulceration, which ultimately led to discontinuing treatment of photoimmunotherapy. In March of 2021, she was referred to dermatology and shave biopsy was performed which resulted in a predominantly plasma cell infiltrate. She was diagnosed with grade 3 severe mucositis and was started on high dose prednisone 50 mg for 5 days with taper. She did note some improvement with prednisone, and the lesions were thought to be autoimmune in nature. However, it did not resolve her symptoms and it was thought that this was a lichenoid drug reaction due to pembrolizumab. Due to the severity of the lesions, she had difficulty with maintaining adequate oral intake and she ultimately required placement of a percutaneous endoscopic gastrostomy (PEG) tube. Attempts were made to taper her steroids; however, each time tapering was attempted she had an increase in symptoms. She was referred back to dermatology for alternative treatment in May of 2021, and concern was raised for possible paraneoplastic pemphigus. Her treatment regimen was planned to transition from steroids to IVIG. She began receiving IVIG 20g in June 2021 on every 4-week infusion schedule, and attempts were made to taper her steroids. She had some improvement, but was not able to taper off steroids without consequently having an increase in symptoms. Ultimately, in November 2021, she was found to have an elevated Envoplakin, confirming a paraneoplastic pemphigus diagnosis. Also, elevated levels of BP180 and BP230 were noted confirming a case of bullous pemphigoid. Her treatment was changed with the addition of rituximab.
The addition of rituximab 1000 mg began in January of 2022 and IVIG was continued along with it. This change allowed for the patient to begin to successfully taper off her steroids. Additionally, she reported improvement in her symptoms. This improvement allowed her to begin to tolerate oral intake. While she had been able to taper off steroids with her current regimen, she is still reliant on her PEG tube for over 90% of her nutrition. At present she remains on IVIG and receives rituximab infusions supplemented as needed which has led to significant improvement in her symptoms. However, she continues to battle flares necessitating courses of prednisone.
She represented to our practice in November of 2022 for further dental extractions of her lower incisors due to localized severe chronic periodontitis of her mandibular teeth. Due to this, her remaining mandibular anterior teeth were indicated for extraction. Due to previously completing hyperbaric oxygen in preparation for previous extractions, she did not undergo further dives prior to extractions. She subsequently underwent extractions and at that time had biopsies of the soft tissues and bone. She ultimately healed uneventfully without complications. In an effort to help improve her oral intake, she is being treatment planned for possible dental implants to support a fixed prosthesis. Unfortunately, due to continued ongoing flares of paraneoplastic pemphigus, further surgical treatment will be delayed until symptoms resolve to limit potential for wound healing complications.
These photos represent the development of the ulcerative mucocutaneous lesions of the lip, tongue, and oral cavity following initiation of pembrolizumab and Photodynamic Therapy. These photos follow the course of the patient’s treatment with prednisone, as well as rituximab showing near resolution.


Squamous cell carcinoma of the head and neck is a challenging disease to treat, which can have significant morbidity associated with its treatment. As presented in this case, the standard approach to this disease is with surgical resection of the associated lesion. Therefore, tissue sparing therapies that can attempt to maximize patient functioning are under active investigation [5]. After multiple recurrences of squamous cell carcinoma, this patient was ultimately enrolled and treated under the protocol of a clinical trial of photodynamic therapy and immunotherapy with pembrolizumab [18]. This patient unfortunately suffered a significant adverse reaction and developed a case of paraneoplastic pemphigus paired with bullous pemphigoid. Paraneoplastic pemphigus is a disease that, although most commonly seen in hematologic malignancies, has been observed in epithelial origin cancers, and several case reports have highlighted an association with pembrolizumab. As in this case the onset of the lesions began with her undergoing photoimmunotherapy. In our case, the time course makes it difficult to point to the cause as both immunotherapy and photodynamic therapy were both started and stopped in short order with each other. Upon diagnosis with detection of elevated Envoplakin and BP-180 and 230, and treatment with rituximab, she was able to see significant resolution in the lesions and was able to once again resume some oral intake, however limited [19,20]. It is important to note that this patient remains PEG tube dependent for most of her nutrition. Unfortunately, this adverse effect of treatment has had a significant negative effect on her quality of life. This brings us to a question of ethics in that, yes, the patient is alive, but at what cost? A decision was made that did allow the patient to continue her life, but the severe complications she met is along the way led to a life significantly altered. This abrupt change for her has been secondary to the development of paraneoplastic pemphigus, rather than secondary to recurrent cancer treatment. Other case reports have demonstrated that patients have had significant reactions with the use of pembrolizumab with other non-hematologic cancers including cases of cutaneous squamous cell carcinoma, ovarian adenocarcinoma, and urothelial carcinoma [13-15].
In conclusion, due to these findings, it can be thought that pembrolizumab likely led to the development or exacerbation of this condition. Although its symptoms can be alleviated with rituximab, the patient continues to have altered functioning of her oral cavity. As case reports and case series continue to arise for patients undergoing immunotherapy with immune checkpoint inhibitors, an adverse event of the development of bullous pemphigoid and paraneoplastic pemphigus should be monitored for. Further research should be conducted to discern the effect that immunotherapy may have in the development of bullous pemphigoid and paraneoplastic pemphigus and if photodynamic therapy may also play a role in the development of these diseases.
None
None
None
