Author(s): Giulia Roda*, Silvia Casanova and Enrico Roda
Introduction and Aim: Refractory ulcerative proctitis is defined as the failure of topical and oral 5-aminosalicylate and corticosteroids treatment. Management of refractory proctitis is often challenging. Curcumin was reported to be efficacious in inducing and maintaining remission in patients with ulcerative colitis (UC). We investigated curcumin in patients with refractory ulcerative proctitis, non responder to conventional therapies (rectal 5 aminosalycilate or steroid in combination with oral 5 aminosalycilate, steroid or azathioprine).
Methods: In a randomized, placebo controlled trial, 10 patients were randomly assigned to assume curcumin capsules (3g/die), in a slow release oral formulation and curcumin enema (3g/die) for one month. Ten patients assumed an identical placebo for 1 month. Primary outcome was clinical remission at week 4. Endoscopic and biochemical data were also recorded.
Results: After one month the number of patients achieving clinical remission was significantly higher in the curcumin treated group (p<0.04; OR, 12,5; 95% CI). After 3 months, 80% of patients treated with curcumin were still in remission vs 10% of patients treated with 5 aminosalycilate (p<0.001; OR, 12; 95% CI). Endoscopic remission (Mayo score <=1 was achieved in 60% of patients treated with curcumin and none in the 5 aminosalycilate group. Conclusion: In this pilot study 3 months topical and oral slow released curcumin therapy in combination with 5 aminosalycilate is efficacious in achieving clinical remission in refractory ulcerative proctitis patients.
Results: After one month the number of patients achieving clinical remission was significantly higher in the curcumin treated group (p<0.04; OR, 12,5; 95% CI). After 3 months, 80% of patients treated with curcumin were still in remission vs 10% of patients treated with 5 aminosalycilate (p<0.001; OR, 12; 95% CI). Endoscopic remission (Mayo score <=1 was achieved in 60% of patients treated with curcumin and none in the 5 aminosalycilate group.
Conclusion: In this pilot study 3 months topical and oral slow released curcumin therapy in combination with 5 aminosalycilate is efficacious in achieving clinical remission in refractory ulcerative proctitis patients.
UC is a progressive chronic inflammatory disease of the colon characterized by mucosal inflammation [1]. UC can be classified (according to the Montreal classification) into three different subgroups based on the extent of colorectal inflammation: disease limited to the rectum (E1), involvement up to the splenic flexure (E2), or extension beyond the splenic flexure (E3). Twentyseven to 54% of patients who are initially diagnosed with proctitis (E1) and/ or left-sided colitis (E2) will progress to develop more extensive disease (pancolitis) [2]. Ulcerative proctitis (UP) is defined as UC with inflammation limited to within 12 cm of the anal verge [1]. Recently, Dutch IBD data has shown an increase of UP [3]. Disease extension is one of the important issues in patients with ulcerative proctitis. Treatment with oral 5-ASA has shown to inhibit extension of ulcerative proctitis. Moreover, ulcerative colitis is a progressive disease given the risks of proximal extension, strictures, pseudopolyposis, gut dysmotility, anorectal dysfunction, colectomy, hospitalization, colorectal cancer and disability [1]. Thus, UP is very challenging being responsible for distressing symptoms and alteration of patient quality of life.
The short-term goal of the treatment in UP is to induce remission, whereas long-term goals are to maintain remission and prevent disease extension, progression and disabilities. Topicallyadministered 5-ASA and corticosteroids such as enemas or suppositories, are effective in the treatment of proctitis [1]. The combination of topical and oral 5-ASA and steroids should be considered for escalation of treatment. Refractory or steroiddependent patients may require immunomodulators or biologics. Alternative medicine can be used complementarily such as curcumin [4]. 5-ASA maintenance treatment is indicated in all UC cases to prevent relapse and disease progression.
Curcumin, an active ingredient of the Indian turmeric, has been studied in the past and found to be useful in the treatment of UC when used as an adjuvant along with mesalamine [5,6]. It has demonstrated anti-inflammatory and anti-oxidative properties in cell lines [7]. Curcumin has shown superiority to placebo in mantaining remission in UC patients up to 1 year.
The efficacy of curcumin in inducing remission in refractory UP patients has not yet investigated. The aim of this pilot study is to investigate the efficacy of curcumin as an add-on therapy with 5-ASA in induction of remission in refractory ulcerative proctitis patients
Ten consecutive patients, 6 women and 4 men, aged 23 to 62 years with ulcerative proctitis refractory to conventional therapy who agreed to participate in this study, were randomly assigned to assume curcumin capsules, in a slow release oral formulation (3g/day) plus curcumin enema (3g/day) for one month. Patients were recruited between July 2015 and September 2016.
Ten patients, 5 men and 5 women, aged 20 to 60 were receiving identical dose of placebo in addition to the existing therapy. Refractory ulcerative proctitis was defined as the failure of topical and oral 5-aminosalicylic acid and corticosteroids. If patients were receiving immunomodulators (azathioprine or 6-mercaptopurine), stable dose had to be maintained 1 year before the study
Exclusion criteria were white blood cells abnormalities, comorbidities such as renal or liver disease, Clostridium difficile infection or other infections and pregnant or nursing female. Blood tests for inflammation (C-reactive protein [CRP]) and hemoglobin and sigmoidoscopies at baseline and 3 months later (week12) were performed.
Clinical remission at one month was the primary outcome and was defined as Simple Clinical Colitis Activity Index (SCCAI) <=2; secondary endpoint included rate of endoscopic remission defined as Mayo score drop >=1 to a score of 0 or 1. Adverse events in both study arms were recorded. Clinical remission and endoscopic remission were reassessed at week 12. All patients signed a consent form.
Comparisons between the 2 groups were performed by MannWhitney U test for continuous variables. Odds ratios (ORs) and confidence intervals (CIs) were calculated. P value < 0.05 was considered significant.
After one month (week 4) of treatment, 70% (7 of 10) of patients receiving curcumin achieved clinical remission as compared with 20% of the patients receiving placebo achieving clinical remission (p<0.04; OR, 12,5; 95% CI). (Figure 1)
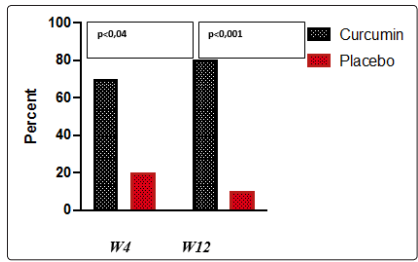
Figure 1: Clinical response at week4 and week12
After 3 months (week12), 80% of patients who had received curcumin were still in clinical remission vs 10% of patients treated with oral and topical 5 aminosalycilates who had received placebo (p<0.001; OR, 12; 95% CI).
Endoscopic evaluation before and after (week12) study treatment was available in 19 patients who gave consent separately (10 patients in the curcumin arm and 9 patients in the placebo arm). Endoscopic remission with a Mayo score <=1 was achieved in 7 of 10 patients (70%) of patients treated with curcumin and none in the 5 aminosalycilate group (p<0.001;OR, 19; 95% CI). (Figure 2)
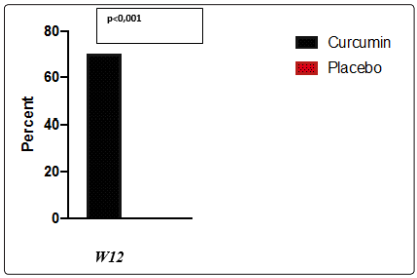
Figure 2: Endoscopic remission at week4 and week12
Four out of patients in the study were treated with immunomodulators
(2 in the curcumin arm and 2 in the placebo arm). There were no
differences in term of outcomes in these patients.
CRP returned to normality after 2 months in 60% of patients in the
treatment arm vs 24% in the placebo arm. There were no changes
in indexes of liver or renal function and in hemoglobin levels.
All the subjects successfully completed the study and no adverse
events were recorded.
Step-up treatment is usually applied for ulcerative proctitis with initial topical 5-ASA followed by a combination of oral and topical 5-ASA. Refractory ulcerative colitis patients to 5-ASA benefit corticosteroids (topical or systemic), followed by treatment with thiopurines and finally treatment with tumor necrosis factor-α (TNF-α) antibodies.
Curcumin possesses immunosuppressive properties via inhibition of IL-2 synthesis as well as IL-2 and mitogen activation of human leukocytes. In murine colitis models, curcumin has been shown to attenuate or prevent DNB or trinitrobenzene sulfonic acid induced colitis by suppressing CD4(+) T-cell infiltration and NH? B activation as well as reducing p38 MAPX activity.
In our preliminary controlled study, we have shown that a 3 months topical and oral slow released curcumin therapy plus 5 aminosalycilate is efficacious in refractory ulcerative proctitis patients. A larger scale, double-blind, placebo controlled trial is needed to further validate curcumin adjuvant effect.
