Author(s): Sara Alshamali *, Jana Alanati, Alessandro Terruzzi, and Rosario Papa
A woman in her 30s, presented with left facial weakness, left eyelid droop, left gaze diplopia as well as right facial and upper limb numbness; which progressively worsened over 1 month. She also developed dizziness, dysphonia, dysphagia, and an imbalanced gait. On exam, she had hoarseness, dysarthria, anisocoria; left pupil miosis, left eyelid ptosis, left gaze diplopia, left lower face weakness, deviation of the palate and uvula towards the left side, right eye nystagmus, right sided facial numbness, right upper limb numbness, right dysmetria, brisk reflexes all-over and an unsteady gait. The work up was positive for OCBs in the CSF analysis and MRI brain revealed a single progressive left medulla oblongata and left cerebellar peduncle hyperintensity lesion. She was diagnosed with and treated for solitary sclerosis with IVMP sessions during pregnancy and then started on Rituximab after delivery which improved her condition
significantly in both clinical and radiological parameters
Central nervous system (CNS) inflammatory demyelinating diseases are a heterogeneous group of disorders. The most common demyelinating disease is multiple sclerosis (MS). It is a chronic inflammatory condition of the CNS that is characterized by demyelination and concomitant axonal and neuronal degeneration [1]. The disease course and phases in MS has variable phenotypes. There are two main phenomena; relapsing-remitting and progressive phenotypes which overlap at different stages in the disease course. Patients could evolve from one step to the other. The disease course classification in MS consists of three phases: the MS high-risk phase, the relapsing-remitting phase, and the progressive phase [2].
We are reporting a solitary sclerosis (SS) case; which is considered a subtype of MS. It is a term used to describe a single demyelinating lesion on magnetic resonance imaging (MRI) that can produce progressive symptoms like primary progressive MS [3]. These solitary demyelinating lesions identified by MRI might be found in the spinal cord, cervico-medullary junction, brainstem, and subcortical white matter [3]. SS patients usually have no clinical symptoms suggestive of relapses affecting other portions of the CNS, and no new lesions found in the patients who had repeat MRI scans of the brain and spinal cord [3]. Oligoclonal bands (OCB) or an elevated immunoglobulin G (IgG) index might present [3,4].
I am reporting this case of SS to share our successful experience in diagnosing such an atypically presenting and challenging case to identify as well as its near complete responsiveness to treatment with Rituximab. Additionally, the phenotypic variability of MS makes it difficult to diagnose such a rarely reported condition; this delays initiating the proper treatment at early stages of the disease which leads to further progression of the condition, associated disabilities, and difficulties in treating the disease at advanced stages. Moreover, the treatment of SS is not well-studied and there are no specific guidelines for choosing disease modifying drugs (DMD). The condition can be approached similarly to progressive MS or based on expert opinion. Finally, there are only a few reported cases which shared their clinical approach; most of them had an unsatisfactory outcome, so it is worth sharing our successful approach to treating SS.
A pregnant woman in her 30s, primigravida at 17 weeks, presented with progressive neurologic symptoms. She first felt numbness around her right mouth that progressed to the right upper limb. She developed left facial weakness, left eyelid droop and diplopia whenever she looked towards the left side. These symptoms were mild and progressed over a course of 1 month. She was also having mild dizziness that got worse over time, nausea, dysphonia, dysphagia to fluid and solid food as well as imbalance and gait disturbance. There were no other neurological symptoms such as confusion, loss of consciousness, blurred vision, changes in colour vision, loss of vision, pain with eye movements, headaches, limbs weakness or seizures.
Review of systems was positive for right hand and foot pain. It was negative for chest pain, palpitations, dyspnoea, cough, dysuria, skin rashes and weight loss
Her past medical history and medications history were positive for hypothyroidism on Thyroxine, colon polyposis on annual colonoscopy and negative for cancer. She reports a negative family history of neurological disorders such as demyelinating diseases or cancers. She is a housewife, a non-smoker and occasionally drinks alcohol. Past surgical and trauma histories were insignificant.
On physical examination, she was alert, oriented to time, place and person with mildly slurred speech and mild hoarseness in her voice. Cranial Nerves exam showed normal visual fields bilaterally. Pupils were round, mildly anisocoric; with miosis of the left pupil, but reactive to light. Right eye nystagmus with fast component beating towards the left in left sided gaze, left eyelid ptosis, diplopia in left gaze and full range extraocular movement.
Right facial sensation was reduced to light touch stimuli. There was left facial muscle weakness of upper motor neuron type. Hearing was normal bilaterally. Palate and uvula moderately deviated towards the left side. Shoulder shrug was strong, and equal bilaterally. Tongue was protruded centrally. Motor exam showed normal bulk, tone, power 5/5 in all 4 limbs with no pronator drift bilaterally. Sensory exam revealed reduction in sensation over the right upper limb, otherwise normal. Reflexes were brisk in all 4 limbs with down going plantars bilaterally. She had mild dysmetria on the right side and an unsteady wobbly gait with tendency to fall towards the right side on the Romberg test.
Her basic laboratory investigations showed normal complete blood count (CBC), liver function tests (LFTs), urea, electrolytes, creatinine, and thyroid function test (TFT).
The stroke work-up was negative for HbA1c, Lipid profile, vasculitis work-up (e.g., ANA, ESR), thrombophilia screen, transthoracic echocardiogram and vessels in MRA.
Other blood samples sent for Quantiferon-TB Gold (QFT), Borrelia in serum and angiotensin- converting enzyme (ACE) were negative. Paraneoplastic markers (e.g., CA 15-3, CA 125, CA 19-9, CAE, AFP tumor marker) were also negative.
She underwent lumbar puncture (LP) for cerebrospinal fluid (CSF) analysis which revealed normal proteins, glucose levels, and WBC levels. Two oligoclonal bands were observed in the CSF, which were not detected in the serum sample. In addition, two paired bands were observed in both the CSF and serum. Other CNS demyelinating disease markers including anti-aquaporin 4 ab and anti-myelin oligodendrocyte glycoprotein (MOG) ab were negative.
CSF: Sample was sent also for onco-neural antibodies (ab); which included anti-Hu ab (ANNA- 1), anti-Ri ab (ANNA-2), anti-Yo ab, anti-CRMP5 ab (CV2), anti-Ma1 ab, anti-Ma2 ab (Ta), antiAmphiphysin ab, anti-Recoverin ab, anti-Tr ab and anti-SOX1 ab were negative.
Other CSF tests were negative for cultures, Borrelia infection, JC virus infection, CSF smear microscopy for acid fast bacilli (AFB) and cytology for malignancy.
MRI Brain: Revealed slight progression of the previously seen T2-weighted and FLAIR hyperintense lesion located in the left side of the medulla oblongata and in the left middle cerebellar peduncle (18.5 mm in height and 14 x 10 mm at its maximum dimension). There was a slight mass effect on the fourth ventricle. No other lesions were seen. No acute or hyperacute ischemic lesion in the DWI sequence. No midline shifts. Normal ventricular system and subarachnoid space. Normal optic chiasm and optic nerve.(Figure 1)
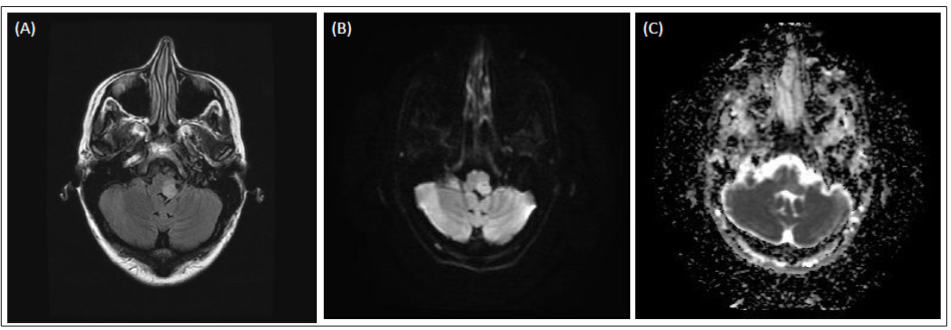
Figure 1: (A, B, C): MRI brain without contrast before IVMP
A. Axial FLAIR MRI image of the brain revealed hyperintense lesion in the left side of the medulla. There was a slight mass effect on the fourth ventricle.
B. Axial DWI MRI image of the brain revealed slightly visible lesion in the left side of the medulla.
C. Axial ADC MRI image of the brain revealed no hypointense lesion in the left side of the medulla.
Revealed hyperintense T2-weighted and FLAIR lesion located on the left in the medulla and in the inferior portion of the left middle cerebellar peduncle on the left side. There was a slight mass effect on the fourth ventricle that was partially compressed. MR spectroscopy centered in the medulla lesion showed a slight increase of choline peak and reduction of NAA and slight increase of lactate compared with contralateral finding. This finding could be referred to as a demyelinating-inflammatory lesion, but it was not possible to exclude a neoplastic lesion.
MRI Cervical Spine: Revealed a subtle cervicothoracic tilt concave to the right with flattened cervical curvature and no significant neurological compromise seen at any level. No intrinsic cord lesion noted as seen in figure 2 (A).
MRI Dorsal Spine: Revealed a mild thoracic scoliosis concave to the left with no significant disc bulge seen at any level. No intrinsic cord lesion noted as seen in figure 2 (B).
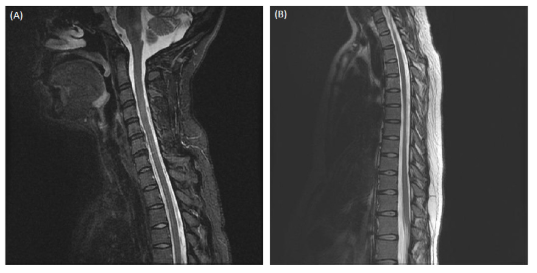
Figure 2: (A, B): MRI cervical spine and dorsal spine without contrast before IVMP
A. Sagittal T2-weighted cervical spine revealed subtle cervicothoracic tilt concave to the right with flattened cervical curvature. No significant neurological compromise seen at any level and on intrinsic cervical cord lesion seen.
B. Sagittal T2-weighted dorsal spine revealed mild mid thoracic tilt concave (scoliosis concave) to the left. No significant disc bulge seen at any level. No intrinsic cord lesion seen.
The patient presented initially to another hospital where she was misdiagnosed as having a stroke based on her first MRI brain and MRA findings. She was started on aspirin despite no cardiovascular risk factors being identified by stroke work-up.
The diagnosis was revised at our hospital as the onset of her symptoms was subacute, progressing over time rather than being sudden acute neurologic deficits of the cerebrovascular accident pattern. The repeated MRI and MRA one month later in our hospital showed enlargement of the supposed ischemic lesion as compared to the first study done in the other hospital. These findings were against vascular territory infarction: the left vertebral artery and left posterior inferior cerebellar artery (PICA) were intact: the absence of cerebellar involvement; very mild atypical visibility in DWI; hyperintensity in ADC; expanded lesion anteriorly out of PICA vascular territory. The pattern is more suggestive of another etiology. Other vascular causes such as haemorrhagic stroke, hematoma, and CNS vasculitis were less likely and excluded as per laboratory tests and images.
The symptoms were localized to the medulla which raised suspicion of paraneoplastic encephalitis syndromes; brainstem encephalitis in particular. This diagnosis was excluded as she had no encephalopathic symptoms such as altered mental status, memory, seizures, or psychiatric symptoms. Tumours were excluded clinically, her tests were negative for serum paraneoplastic markers, negative for the supportive markers of an autoimmune pathogenesis like encephalitis-specific antibodies and paraneoplastic autoantibody profile in serum and CSF. No CT scan of the chest, abdomen and pelvis was done during the initial work-up as the patient was pregnant in the second trimester.
She was referred to a haematology team to exclude neoplastic etiologies such as a primary CNS lymphoma. It was less likely because of the negative kappa and lambda light chains, CSF cytology/ flow cytometry results and the atypical MRI findings. Biopsy was difficult to be done as she was pregnant at presentation.
The other top differential diagnosis was inflammatory demyelinating CNS disorders like multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM). Considering the pregnancy, contrast was not administered to evaluate the lesion adequately, so MRI Spectroscopy was done, and it was more in favour of a demyelinating lesion than a neoplastic lesion. Although the CSF analysis was positive for OCBs, the 2017 McDonald criteria was not met in terms of dissemination in time and space. In addition to that, brain and spine MRI did not fulfil the 2016 Magnetic Resonance Imaging in Multiple Sclerosis (MAGNIMS) criteria. She had paired CSF and serum bands. This is known as “mirror pattern” which may indicate co-existing systemic immune reaction outside of the CNS with passive transfer of OCBs from the serum to the CSF through an abnormal blood brain barrier and does not indicate local IgG synthesis [5]. Another point to consider is that MS is usually inactive during pregnancy, this patient disease was fully active while she was pregnant making MS less likely the diagnosis.
ADEM was considered due to the presence of progressive new-onset polyfocal neurologic symptoms, but the absence of encephalopathy, temporal relation to infection or vaccination and typical imaging findings of multifocal demyelination lesions excluded it.
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids was down the list of our differential diagnosis (despite responding very well to steroids as described later), because the symptoms localised the lesion to the medulla not the pons and the absence of the characteristic MRI brain findings; multiple punctate contrast enhancing lesions (in this case, imaging with contrast was done after delivery) confined to the pons
Other inflammatory CNS disorders like neuromyelitis optica spectrum disorder, anti-myelin oligodendrocyte glycoprotein syndromes, neuro-sarcoidosis and systemic inflammatory conditions like Behcet’s syndrome were excluded clinically and as per the laboratory tests and images.
CNS infections; viral (e.g., herpes simplex virus, human herpesvirus 6, human immunodeficiency virus, enterovirus), fungal (e.g., cryptococcus), bacterial (e.g., listeria, Whipple disease, neurosyphilis) and mycobacteria (e.g., tuberculosis infection) were also excluded as per the laboratory tests and images.
In view of her pain in multiple joints (right hand and foot), the rheumatology team was counselled. She underwent autoimmunity tests, nerve conduction study of the hands, ultrasound of the wrist,hand and foot, hip joint and pelvis X-ray. There was no evidence of any rheumatological disorders.
Laboratory tests were also sent for vitamin B-12, thiamine, folic acid, toxic screening looking for possible nutritional deficiency, toxic and metabolic etiologies. All these tests were negative.
She was diagnosed with clinically isolated syndrome (CIS); its subtype solitary sclerosis (SS) in particular [2]. CIS is a term refers to a mono-symptomatic attack that does not fulfill diagnostic criteria for MS but may predispose to clinically definite MS [3]. She was planned for further monitoring of her symptoms clinically and by follow up brain and cervical spine MRI images with contrast after delivery; looking for possible new lesions to rule out dissemination in time and space and clues for other diagnosis.
She was treated with intravenous methylprednisolone (IVMP). It was started around 1 month after the onset of her symptoms (as soon as she presented to our hospital). She was in her second trimester at that time. She did not improve neither clinically nor radiologically. The follow up brain MRI 1 month after the first IVMP course revealed minor progression of the lesion in the left medulla oblongata; it measured 19.5 mm in height and 16 x 10 mm at its maximum dimension. So, she was given repetitive, monthly courses of IVMP throughout her pregnancy. She received a total of five courses, 3 days each of 1 g IVMP.
She started noticing gradual improvements after the 2nd and 3rd sessions of IVMP. She no longer had miosis. She reported an improvement in the dizziness, diplopia, dysarthria, dysphagia, and facial deficit. However, she showed moderate palatal deviation towards the left side and she was still unable to walk independently. She complained of severe right sided numbness and left eye ptosis. The brain MRI revealed a slight reduction in the size of the lesion located in the medulla oblongata and mid cerebellar peduncle on the left side as seen in figure 3.
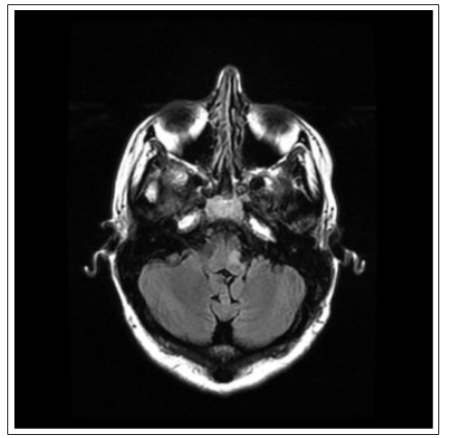
Figure 3: MRI brain without contrast after five courses of IVMP, before delivery Axial FLAIR MRI image of the brain revealed a slight reduction in size of the lesion located in the medulla oblongata and in the left mid cerebral peduncle. The maximum diameter in the coronal 3D FLAIR was around 10.8 mm (about 0.43 in); less than the measurement in the MRI done before this one which was 13.4 mm (about 0.53 in) x 10.6 mm (about 0.42 in). No other obvious intraparenchymal brain lesions were seen.
She underwent MRI brain and cervical spine with contrast and brain F-fluorodeoxyglucose positron emission tomography (FDG-PET) 1 month after delivery for further evaluation of the previous lesion, for possible new lesions and to consider biopsy for diagnosis confirmation.
The MRI brain with contrast showed a reduction in size of the left medulla oblongata and the left middle cerebral peduncle lesion. T1-weighted post contrast sequence showed slight enhancement in the left middle cerebral peduncle as seen in figure 4. There were no obvious changes or new lesions in the cervical spine.
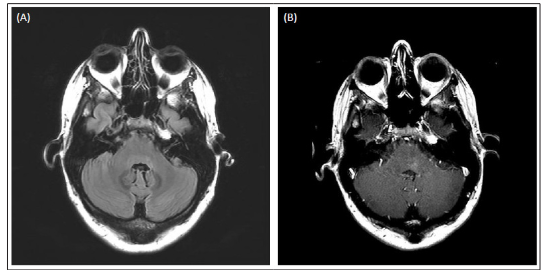
Figure 4: (A, B): MRI brain with contrast after delivery, received 5 courses of IVMP and before starting Rituximab
A. Axial FLAIR MRI image of the brain revealed a reduction in size of the lesion located in the medulla oblongata and persistent hyperintense lesion in the left middle cerebral peduncle around the IV ventricle
B. Axial T1-weighted post contrast MRI image of the brain revealed enhancing lesion in the left middle cerebellar peduncle near to the IV ventricle. There was no mass effect on the fourth ventricle. No other lesions were seen. Normal brain parenchyma in the supratentorial region.
The lesion seen in the MRI brain had become smaller in size because of the IVMP effect making biopsy difficult to be performed; furthermore, the risk of post-surgical complications would outweigh its benefits.
Brain FDG-PET and whole-body PET CT imaging revealed no clear evidence of hyper or hypometabolic activity in the previously mentioned lesion or elsewhere in the brain. No other evidence in the rest of the body of FDG avid malignancy was noted.
Rituximab was started as an immunomodulator treatment 3 months after delivery. She received weekly intravenous Rituximab 500 mg, for 4 weeks, with pre-medications including intravenous Diphenhydramine 25 mg IV, intravenous Methylprednisolone 250 mg and intravenous paracetamol IV 1000 mg as needed for pain or fever. She tolerated the treatment with no side effects. She had received another 2 courses of Rituximab IV infusion of the 1000 mg dose, 2 sessions at 2 weeks intervals, every 6 months.
She also received symptomatic treatments such as Pregabalin, Gabapentin and Duloxetine for numbness. She got physiotherapy sessions for gait and balance training. She was treated for major depressive disorder with Vortioxetine.
She showed further clinical and radiological improvement with Rituximab in terms of less numbness, normalized voice pitch, no dysphagia, only mild diplopia on extreme left gaze, improved balance, and gait.
The latest examination around 1 year after receiving Rituximab showed normal neurological examination except for mild diplopia on extreme left gaze, mild reduction in sensation around the right angle of the mouth and right upper limb. She underwent a left eyelid surgery to lift it as ptosis failed to improve.
The latest MRI brain around 1 year after receiving Rituximab revealed an almost complete disappearance of the left middle cerebellar peduncle lesion with no enhancement as seen in figure 5. The follow up cervical spine MRI revealed no lesion in the cervical spinal cord.
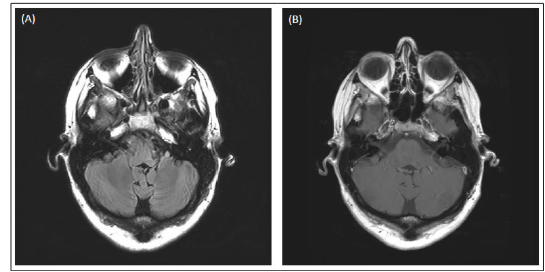
Figure 5: (A, B): MRI Brain with contrast 1 year after receiving Rituximab
A. Axial FLAIR MRI image of the brain revealed almost complete disappearance of the previous hyperintensity lesion located in the left medulla oblongata and the left middle cerebellar peduncle.
B. Axial T1-weighted post contrast MRI image of the brain revealed resolution of the enhancement previously seen in the left middle cerebellar peduncle lesion. The lesion in the left middle cerebellar peduncle had almost completely disappeared.
The future treatment plan includes getting Rituximab, MRI brain and spine every 6-12 months. She is undergoing regular IgG/IgM testing in serum and FBC to rule out leukopenia or thrombocytopenia to avoid excessive immunosuppression and side effects of anti CD20.
She stopped the symptomatic treatments with Pregabalin, Gabapentin and Duloxetine for numbness despite some improvement, because the numbness can be extremely painful at times, as well as she suffered the medications side effects such as weight gain, so it was no longer worthwhile taking these medications. She remains on Vortioxetine for major depressive disorder.
The term solitary sclerosis (SS) has been used to describe spinal cord and brainstem lesions that result in progressive long tract and myelopathic features in combination with CSF abnormalities [4-6].
SS is a term that defines patients whose imaging findings at the time of CIS do not fulfill the minimum MRI requirement for an MS diagnosis, but the existing “multiple” additional CNS lesions are unexplained by other pathology and are typical of MS in location, orientation, and shape. When a patient with SS proceeds to fulfill the minimum MRI requirement for an MS diagnosis (at least three of the four imaging criteria), the diagnosis of singleattack MS may be used [2].
Another concept should be described to understand the SS phase. When a patient presents with symptoms not typical of MS and an MRI is obtained that fulfills the diagnostic imaging criteria, a diagnosis of radiologically isolated syndrome (RIS) is given. When these patients develop their first MS symptom, they fulfill the criteria for single-attack MS. There are many asymptomatic individuals present with lesions typical for MS but do not fulfill the diagnostic imaging criteria. The term pre-radiologically isolated syndrome (Pre-RIS) is used by some to define such cases. These individuals with Pre-RIS might evolve to having RIS when they fulfill the imaging criteria or evolve into having SS when they develop their first clinical event [2].
If SS leads to a progressive phase, it is described as progressive solitary sclerosis (PSS) [2]. This condition follows a course similar to primary progressive MS but lack the dissemination in space required to fulfill MS criteria [7].
Further understanding of the pathophysiology of this entity and whether it could be incorporated into the primary progressive MS phenotype requires further research and discussion [7]. The treatment of progressive solitary sclerosis is not well-studied but can be approached in the same manner as primary progressive MS [8].
Our case presented with subacute, progressive brainstem symptoms of left facial weakness, left diplopia, right sided numbness and right dysmetria. The age at onset was similar to that of patients with MS. MRI brain revealed a single left sided medulla oblongata lesion with minor contrast enhancement in favour of demyelinating lesion. Dissemination in time and space were not met by clinical or radiological findings. She had abnormal CSF findings; a borderline positive OB in CSF (2 bands), which supported a demyelinating process [9]. In view of negative paraneoplastic, onconeural antibodies, MR Spectroscopy, FDG-PET and vasculitis panel, she was diagnosed with SS. The condition was responsive to IVMP and with Rituximab. The response of the condition to the treatment proved our thought of demyelinating process. She had a first-ever progressive event. The clinical phenotype was similar to those of either primary progressive or single-attack progressive MS. She did not experience a second clinical relapse; hence, she did not evolve into clinically definite relapsing-remitting MS.
There are few published case reports as SS with variable presentations; dysarthria, diplopia, myelopathy and gradual motor impairment [10-13]. A similar case to ours was reported about a patient who presented with brainstem symptoms; paroxysmal dysarthria and dizziness, MRI brain revealed hyperintensity in the caudal midbrain, positive CSF analysis for OCBs and unrevealing PET scan. The patient received high dose IVMP, his symptoms completely resolved and the lesion showed improvement in the repeated brain MRI [10].
Another case of a young female patient with brainstem symptoms. She presented with diplopia with full recovery with oral steroids, followed by progressive quadriparesis and dysarthria over years due to a single pontomedullary lesion in the MRI. The CSF test in this case was negative for OCBs. Despite experiencing clinical deterioration over time, the MRI lesion was the same without evidence of dissemination in time and space, hence she was diagnosed with PSS. She also received IVMP, plasmapheresis and rituximab. Unfortunately, the disease course was progressive. She partially improved after adding cyclophosphamide [11].
A few case series were reviewed, reporting patients with progressive myelopathy and progressive motor impairment [12-14]. In addition to sharing similar characteristics of the previously mentioned cases such as single radiologically identified CNS lesion, elevated IgG index and/or oligoclonal bands in the CSF studies, no relapses and no other explained differential diagnosis; evoked potentials were examined, looking for possibility of dissemination in space. These tests were normal in the majority of the cases. As in other progressive subtypes of MS, immunosuppressive and immunomodulatory therapies with IVMP, cyclophosphamide, azathioprine, therapeutic plasma exchange, mitoxantrone, natalizumab, glatiramer acetate, interferon and methotrexate did not appear to alter the ongoing worsening of neurologic deficits in two case series [12,13]. On the other hand, the chronic progressive course stopped during follow-up in another case series [14].
Brain biopsy of a patient showed demyelination, chronic inflammation, and gliosis without evidence of a neoplasm. Another patient had an autopsy that revealed a solitary demyelinating lesion with profound myelin loss and relative axonal preservation in the rostral pontine tegmentum.(13)
Solitary sclerosis is a challenging diagnosis.
Dr. Sara Alshamali is the main author who wrote the manuscript, edited, and submitted the article. Dr. Jana Alanati participated in collecting the investigations data of the patients and addressed revision to the manuscript. Dr. Alessandro Terruzzi is the most responsible physician who was involved in direct medical care and revised the manuscript for content. Dr. Rosario Papa provided the MRI images. We are thankful to the patient for consenting to publish her case.
