Author(s): Suárez-Vargas Daniel, Franco-Lugo Desireé, Rey-Valadez Roberto, Mena-Guerrero Tamara and Cueto-García Jorge*
Importance: A new successful therapeutic option for chronic complicated pressure lesions using a Carbohydrate Polymer with Zinc Oxide (CPZO®).
Introduction: A 20-year-old male patient diagnosed with congenital Myelomeningocele was seen and examined in our office on December 08, 2014. When we first received the patient, he had two very large fistulized pressure ulcers stage IV in the gluteal and perianal areas. Both ulcers presented evidence of infection, with purulent fecal discharge, and extensive inflammation and destruction of surrounding tissue.
Conclusions and Relevance: This case proves the therapeutic efficiency of CPZO® a new Medical Device II with pro- healing, anti-inflammatory and bactericidal properties on a young male patient with chronic complicated severe pressure ulcers.
AGG, a 20-year-old male patient diagnosed with congenital Myelomeningocele, whose mother informed us that since birth, he had been treated at Teleton , was seen and examined in our office on December 08, 2014. On physical examination, two stage IV fistulized pressure ulcers were found in the posterior sacral and gluteal areas, being the diameter of the longest >22 cm in length. Both presented evidence of infection, with purulent fecal discharge and extensive destruction of surrounding tissue (Figure 1).

Figure1: Two-stage IV fistulized chronic pressure ulcers can be seen in the posterior sacral and gluteal areas. Both showed purulent discharge and extensive necrosis.
The patient had been previously treated in two of the largest social security institutions, where he received care for 13 months through several hospitalizations. His family reported that previous treatments included multiple surgical debridements of the wound, local and systemic antibiotic therapies, even using fluoroquinolones applied intravenously; two different sessions of skin grafting were carried out under local anesthesia which failed to improve the ulcers.
For compassionate reasons, the gravity of the patient’s problem and its management were carefully explained to his parents to obtain their informed consent, and the treatment was started.
The patient was treated with daily topical application of a Carbohydrate Polymer with Zinc Oxide (*Pebisut ®, CPZO ) applied directly by the mother on the ulcers after his daily baths (Figure 2) waiting 2-3 minutes for complete dermal penetration and then covering it with a petrolatum gauze. The TIME protocol was continuously used to assess the presence of necrotic tissue, infection, inflammation, moisture and epithelial cicatrization of the wound [1].

Figure 2: CPZO treatment being applied directly to the wound and then covered with a petrolatum gauze.
The patient was initially seen in the office every two weeks until the mother informed us about the healing of the ulcers.
At the end of the first month of treatment, the ulcers were no longer fistulized and showed a 60% healing.
Finally, three months after starting the treatment, the patient presented 100% healing of both ulcers (Figure 3), treated with a total of 4 jars (30 g. each) of CPZO.
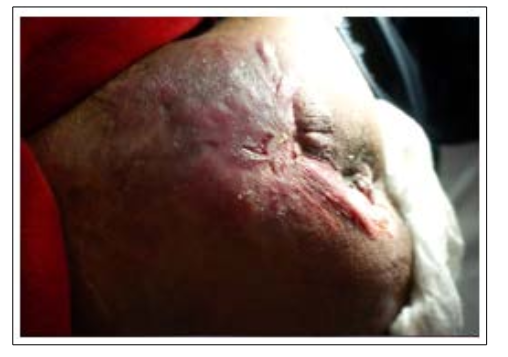
Figure 3: CPZO treatment applied locally for 3 months. Both ulcers are 100% healed.
Neural tube defects are malformations that cause several life threatening pathologies of these patients, such as the case reviewed in this paper. Recent reports in the literature show that the prevalence of neural tube defects is 4.7 cases per 10,000 live births [2,3]. Myelomeningocele is a congenital malformation presented due to incomplete closure of the neural tube that results in exposed neural tissue. These patients have a permanent disability, being paraplegia the most important and problematic that results in several thoracic and lumbosacral lesions [4,5]. The inability of the patient to move, and the hypoesthesia frequently lead to complications such as pressure ulcers [6]. These lesions destroy superficial and deep tissues and structures with ischaemia and necrosis and in stage IV affect the bones and pelvic organs and produce systemic septic complications with elevated morbidity and higher mortality rate [7-9].
Risk factors such as poverty and advanced age increase the morbidity and mortality of the disease. On the other hand, geriatric patients who suffer from pressure ulcers have bladder and renal complications that lead to constipation, incontinence and severe infections, which gradually deteriorate their life condition [10,11]. Early detection and prevention of these complications can produce a reduction in their gravity and thus also reduce the economic impact, and may improve the prognosis. The impact for the family was not only emotional, but also economic due to the “out-of-pocket” expenses incurred by being forced to buy many of the prescribed medications and antibiotics. Patients with pressure ulcers that have a constant change of position, special mattresses and strict full time care provided by nurses and their own families such as the mother in this case, can prevent potentially fatal results and therefore it is important to emphasize that prevention is the most important part of the treatment that these patients should receive [8-12].
Vela’s paper (12,13) shows the latest national epidemiological data about pressure ulcers in Mexico, concluding that the prevalence is 12.92% being the frequency as follows: sacrum= 27%, heel= 27%, ischium= 10%, head= 4%, and elbows= 3% [6]. Besides this, the latest guidelines (2018) establish that the treatment for pressure ulcers in patients with stage II, III or IV ulcers must include wound cleansing, debridement of necrotic tissue, administration of systemic antibiotic treatment when needed, as well as nutritional support, glycemic control, and pain management [4,9]. Our patient presented with two very large stage IV ulcers as a complication of uncontrolled diarrhea that lasted for more than ten days.
These lesions could have been fatal due to systemic infection and malnutrition, without mentioning the increase of the overall cost.
Our patient had previous ineffective treatments carried out in two very large social security institutions where he received 13 months of antibiotic therapy, among other procedures, standing out the usage of quinolones [14]. It’s important to emphasize that chronic antibiotic therapy is reported to be one of the major risk factors to develop antibiotic bacterial resistance (14), as well as lower functional status, which is the case of our patient.
According to a recent nursing journal (9), medical units specialized in the treatment of pressure ulcers (PU) account for an estimate of USD132,758.82 for ambulatory care and USD 35,878,481.15 for hospital care, per month to public institutions in Mexico [6,8]. From a socio- economic point of view, these kinds of expenses produced damage to the family’s economy and therefore damage to their quality of life. The complete treatment of this patient in an ambulatory setting, using CPZO had a cost estimated at USD700 which indicated very important savings that could be applied in large institutions as well [15-18].
Although antibiotic therapy can be an important treatment for pressure ulcers when needed, it is important to be aware that nowadays, we are dealing with a new emerging world problem, namely multiple drug resistance to antibiotics. Such infections have become more and more common and are increasing in morbidity and mortality. The groups of microorganisms that usually affect pressure ulcer wounds are Staphylococcus epidermidis, Enterococcus, Streptococcus and Corynebacterium. Being Staphylococcus aureus and Pseudomonas aeruginosas the most common bacterias in pressure ulcers [19-21].
We have demonstrated that the use of a non-antibiotic medical device II CPZO, a locally-applied polymer combined with zinc oxide treatment, successfully healed these chronic fistulized ulcers due to its bactericidal and anti-inflammatory properties. ZnO is already used in various dermatological treatments because its nanoparticles have shown a 20-60% biofilm reduction of Gram-positive bacteria [22-24]. But in combination with a carbohydrate polymer (CPZO), produces lower chemotaxis of inflammatory cells to the stimuli with CCL2, CCL5, and CXCL12 chemokines, resulting in a lower infiltrate of macrophages and lymphocytes [25-27].
The Carbohydrate Polymer with Zinc Oxide (CPZO), has shown potent bactericidal and anti-inflammatory properties that enhance the wound-healing process, as shown in its initial clinical evaluation. The use of this medical device therefore can be applied in the treatment of diabetic ulcers, chronic varicose venous ulcers and other chronic wounds. CPZO is well tolerated, has not produced any undesirable effects, is easy to prepare and apply at home and does not require refrigeration for storage nor transportation [27-30].
The patient presented herein with 2 chronic very large pelvic-perineal fistulized pressure ulcers, complications of Myelomeningocele, with failure of previous different treatments. CPZO, a Carbohydrate Polymer with Zinc Oxide as a sole treatment for 14 weeks, achieved complete healing of both lesions. Due to its therapeutic and many other advantages, CPZO could be considered as a first line therapeutic option in treating chronic complicated ulcers.
None reported.
