Author(s): Hani Raoul Khouzam
Obstructive sleep apnea (OSA)is a type of sleep-related breathing disorders which is associated with frequent awakenings leading to sleep fragmentation. Posttraumatic stress disorder (PTSD) is a psychiatric disorder that is also associated with sleep fragmentation and disruption. A possible link between OSA and PTSD needs to be accurately identified in patients who present with either OSA or PTSD. This article will review the diagnostic criteria of OSA and PTSD, the proposed link between these two distinct clinical entities and the treatment interventions for both disorders. The accurate identification and appropriate treatment of OSA and PTSD would ultimately prevent sleep disruption and its serious medical and mental complications, leading to improved functioning in patients whose lives are adversely impacted by these disabling medical and mental disorders.
Posttraumatic stress disorder (PTSD) is one of the mental health disorders where sleep disruption is among is distinctive diagnostic criteria [1]. Sleep problems are a component of PTSD arousal symptoms, and if they are not promptly treated, overtime they acquire their own intensity and progression and eventually contributing to the disabling effects of the disorder [2]. Although insomnia and nightmares have been the most prominent sleep problems that are frequently associated with PTSD,emerging trends in clinical practice, have shown a probable link between sleep difficulties in obstructive sleep apnea (OSA)and in PTSD [3,4].The appropriate identification and management of OSA as an integral component of the overall treatment of PTSD and vice versa would lead to the restoration of wellness for patients who have these two cooccurring serious mental and medical disabling conditions and eventually resulting in a notable improvement in their quality of life.
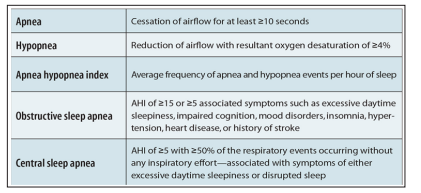
OSA is a type of sleep-related breathing disorders as outlined in Table 1 and is characterized by recurrent episodes of partial and complete airway obstructions during sleep resulting into repetitive apneas and hypopneas. The disease severity is measured using the apnea-hypopnea index (AHI), i.e., the mean number of apneas and hypopneas per hour of sleep. OSA is defined when the AHI is ?5 and OSA syndrome when AHI ?5 is accompanied with daytime sleepiness. The American Association of Sleep Medicine defined daytime sleepiness as mild, moderate, and severe in relation to impact on social life during the daytime [5]. The Epworth Sleepiness Scale (ESS) is, the most often used measure to define daytime sleepiness [6]. Several medical conditions have been associated with OSA including hypertension, coronary artery disease, stroke, and type 2 diabetes [7]. Individuals who develop OSA before age 70 also have an increased risk of early death [8].
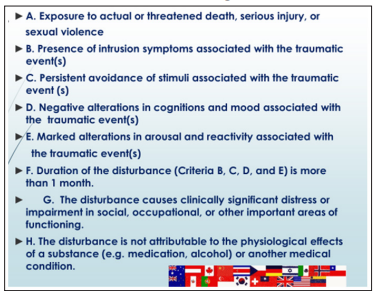
As a psychiatric condition PTSD develops following a traumatic event that involves physical harm that has been experienced, threated with, or witnessed toward self, loved ones or others. It is characterized by recurrent and intrusive distressing recollections of the traumatic events and is associated with a sense of reliving the experience with intense psychological or physiologicaldistress at exposure to cues that resemble the traumatic event, avoidance of stimuli associated with the trauma, or inability to recall important aspects of the trauma [1]. Individuals with PTSD often experience a cluster of additional symptoms including loss of interest, estrangement from others, sleep disturbances, nightmares, irritability, difficulty concentrating, hypervigilance, exaggerated startle responses, aggressive behaviors, shame and guilt, and some patients develop dissociative flashback episodes [1,9]. Typical examples of traumatic experiences that may predispose to PTSD include sexual assault, military combat, mass conflict and displacement, and life-threatening physical illness [10]. The diagnostic Criteria of PTSD according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), are summarized in Table 2 with the addition of flags of various countries to demonstrate the global and worldwide scope of this human condition.
It is estimated that OSA affects between 17 to 22% of the general population [11]. Individuals with PTSD have higher incidence of OSA ranging from 12 to 90% [12]. Additionally, the co-occurrence of OSA and PTSD is more likely associated with increased PTSD symptoms severity [13]. Left untreated, OSA can lead to the development of serious chronic medical conditions such as type 2 diabetes, cardiovascular disease, stroke, hypertension heart failure, dementia, and certain type of cancers [7,14,15], thus further aggravating preexisting PTSD. Untreated OSA can also lead to neurocognitive deficits and the development of other psychiatric disorders and substance abuse which can lead to worsening severity of PTSD symptoms [16,17]. Survivors of fire, victims of consecutive crimes, and to a greater extent the veterans’ population with PTSD also experience worsening of OSA [18,19]. Among the general population, the risk for OSA increases with age, however, young veterans with PTSD may have a higher OSA risk for their age group [20]. Individuals with PTSD and OSA are more likely to experience recurrence of severe depression, a higher suicide risk, increased incidence of substance abuse, and a poorer quality of life [21].
A dysfunction in the hypothalamic-pituitary-adrenal (HPA) axis and decreased hippocampus volume have been postulated as underlying possible factors for the link between sleep -related breathing disorder and PTSD [22]. Changes in the functioning of the HPA axis have also been reported to be associated with PTSD [22,23]. Additionally, growth hormone (GH) levels are reported to be lower in some patients with PTSD compared with healthy control subjects [24]. The reduction in GH secretion is also correlated with night awakenings and affects synaptic plasticity, thus contributing to the prolongation of recovery and further perpetuation of PTSD symptomatology [18]. The frequent awakenings due to OSA lead to sleep fragmentation during the rapid eye movement (REM) sleep stage causing interruption of memory consolidation and preventing fear extinction [25,26]. The proposed interactions between OSA and PTSD is illustrated in figure 1 [27].

GH=growth hormone; HPA=hypothalamic-pituitary-adrenal;
OSA=obstructive sleep apnea.
Copyright 2015 by the American Thoracic Society
The hypervigilance and heightened alertness in patients with PTSD may contribute to the development of OSA [28]. It is possible that certain patients with PTSD who experience sleep difficulties due to nightmares recurrence have increased sleep fragmentation that could predispose them to develop OSA [18].
Continuous positive airway pressure (CPAP) as illustrated in figure 2, remains the mainstay of therapy for OSA. It exerts its beneficial effects by acting as a pneumatic splint to prevent the upper airway soft tissue from collapsing. Other effects include a change in the upper airway muscle tone and increasing functional residual capacity [29]. In some patients with PTSD, CPAP therapy has been associated with a dramatic improvement in sleep quality, reduction in nightmare frequency and severity as well as a decrease in daytime sleepiness [30]. Despite the overall improvement in PTSD symptomatology with CPAP therapy, there is a significant decrease in treatment adherence in patients with PTSD compared to the general population with OSA [30,31]. Several factors could contribute to the difficulty in adherence with CPAP therapy in patients with PTSD, such as mask discomfort, claustrophobia, and air hunger [32]. Clinicians may need to consider adjunc-tive interventions to improve CPAP adherence such as cognitive behavioral therapy [33]. Providing oral appliances, and nasal expiratory positive airway pressure may be also be considered to improve treatment adherence [33].
The effective treatment of PTSD requires a comprehensive approach that incorporate the management of co-occurring medical, psychiatric, and substance use disorders concurrently with PTSD [34]. Pharmacotherapy is often necessary. Though the US Food and Drug Administration (FDA) only approved two antidepressants, sertraline and paroxetine, for the pharmacological treatment of PTSD, many patients do not respond to these and may need combination of medications, such as other antidepressants, antiadrenergic agents, anticonvulsants/mood stabilizers, and atypical or second generation antipsychotics [35]. The pharmacological treatment of PTSD is geared toward the alleviation of the various symptom clusters including intrusion, avoidance, negative alterations in cognitions and mood, and the alterations in arousal and reactivity [36]. Nonpharmacological intervention and psychotherapy are important as well with prolonged exposure and cognitive processing therapy as the two main trauma-focused psychotherapies with the strongest evidence base for the treatment of PTSD [37]. Social and spiritual intervention and the inclusion of families, friends, and significant others are of integral importance for the successful overall management of PTSD, especially in those patients who are experiencing the associated symptoms of social avoidance, interpersonal isolation, survivor guilt, and those who are at a high risk of suicide [38].
The link between OSA and PTSD have been proposed due to their common and overlapping clinical features. These two distinct conditions if left untreated, have a detrimental effect on the maintenance of normal sleep patterns, affecting daytime functioning and quality of life. Both disorders seem to affect and perpetuate each other, creating persistence of sleep difficulties. Sleep fragmentation and disruptions have serious medical and mental complications. Clinicians are strongly advised and urged to consider OSA as an undiagnosed entity in patients with PTSD and vice versa to explore the possibility of PTSD as a confounding factor contributing to the frequent awakening associated with OSA. Treatment options include CPAP therapy for OSA and both pharmacologic and nonpharmacological interventions in PTSD .An astute assessment and management of OSA and PTSD despite its inherent difficulties and challenges will ultimately lead to improved sleep, remission of disabling symptoms and restoration of daily functioning and quality of life

Sincere appreciation to Drs, Nabil R L Bechai and Avak A. Howsepian for their support and my gratitude and thankfulness to my wife Lynn and children, Andrea and her husband Nic, and their daughter Abigail , Andrew and Adam, my sisters Hoda and Héla, and my brother Hadi and cousin Mona for their encouragement.
