Author(s): Mahendra Patait*, Arjun Shetty, Bikash Pattanaik, Sameer Narkhede, Shrinivas Ambarkar and Ashok Mathew
Three-dimensional imaging, particularly cone-beam computed tomography (CBCT), has made significant contributions to the planning and placement of implants of missing tooth or at immediately removed tooth. The accuracy of CBCT data can be used to fabricate a surgical guide that transfers the implant planning information to the surgical site to facilitate implant placement. Prosthetically driven implant prosthesis assures good aesthetics, function and more importantly hygiene maintenance enabling long time success. Accuracy in treatment planning and implementation of planned treatment is vital for this success.
Here we describe a method for applying CBCT data to aid in the planning and placement of implant using CBCT data to aid in planning and placement of Missing and immediate extracted tooth implant.
By actual standard for care for replacement of missing tooth by means of implants expects not only the replacement of missing teeth in terms of function, but also the achievement of satisfactory aesthetics [1]. Optimal positioning of the implant through prosthetically driven decision-making is mandatory to achieve these goals [2,3].
Computer-aided methods may offer significant advantages in the treatment planning and help clinicians to perform successful implant placement while avoiding elevation of large mucoperiosteal flaps or eliminating them at all, causing less pain and discomfort to patients.
Patients can benefit from having painless, flapless implant replacement with missing teeth immediately. However, to achieve such results in the implant-based replacement need a carefully planning in advance. The routine conventional freehand implant placement is challenged by many of the factors to obtain the beneficiary results. Some of them are patient movement during drilling, a limited arial vision of the operative field which is mostly limited to the edentulous soft tissues in the area of concern, accurate diagnosing the surgical site surface on 2 Dimensional X Ray interpretation and transfer of 3 dimension radiograph into the actual surgical environment and Integration of aesthetic, biomechanical and functional constrict.. Thus the maxillofacial radiologist has to take numerous decisions with the consultation of implantology and virtual planning ranging from surgical aspect to the implant positioning in a critical time period.
A thorough preoperative planning done by Oral radiologist with the view point of accurate placement of Dental Implant will clear the surgeons mind allowing more time to concentrate on the patient and tissue handling.
The growing interest in flapless minimally invasive implant placement with the option of pre-fabricated temporary prosthesis immediately temporary prosthesis to restore function and aesthetics, have led to the development of numerous three-dimensional (3D) visual software programmes.The 3D Visualization of implant placement site characteristics and neighboring anatomy and vital structures provides the clinicians with more clear vision of the surgical, prosthetic and aesthetic requirements of the proper treatment and eventually enhance the decision-making, overall increasing the reliability of the overall dental implant treatment.
Computer-guided imaging dental implant placement needs 3D imaging of both the jaw bone and the planned prosthesis virtually. Such integration of the planned prosthesis within the intraoral dental implant is achieved through a double-scan technique with fiducial marker-based matching means use of gutta-percha incorporated in temporary prosthesis while during the second scan [4].
First, the patient is scanned with the temporary prosthesis in the mouth, stabilized in the proper position by an occlusal silicone index. The planned same prosthesis is than scanned separately, with different exposure parameters suggested by specific guide designing software in order to allow its in order to allow its 3D visual-station in the software. As the markers are visible in both sets of scans, they can be fused and the prosthesis properly positioned within the maxillofa- cial structures. A recently introduced 3D implant planning software (B n B Implant Software ) automatically combines the Digital imaging and communications in medicine (DICOM) data belonging to the CT/CBCT examination of the patient with the STL data derived from the optical digital high- resolution scan of the preoperative patient master cast [5].
Additional benefits of this streamline workflow is visualized more planning options well before the surgery is done. Once the planning is completed and approved by the clinician the digital information is sued to produce the surgical stent or template that will be tooth supported with CAM rapid prototype ( millining or 3D printing) [6,7].
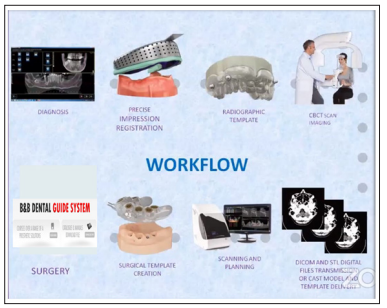
Flow Chart of Digital Designing of Imaging Guided Implantology.
Implant treatment in the aesthetic zone still represent a challenging task for surgical as well as prosthetic phase [8].Potential advantage of a computed guided implant placement in the aesthetic site includes a reduced mucosal recession of maximum preserver of peri implant papillae in case the implant properly positioned.

Figure 1: Extra Oral View of The Planned Patient
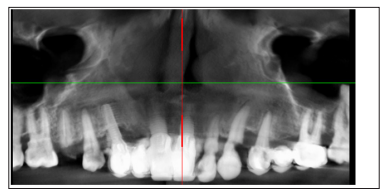
Figure 2: Cone Beam CT of Patient
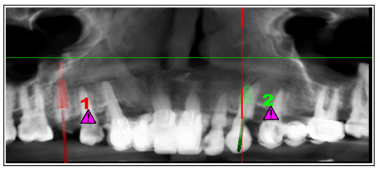
Figure 3: Virtual Implant Planning on DICOM Data
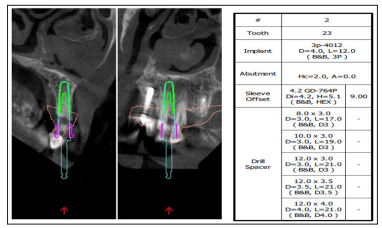
Figure 4: 23 region details of implant and Scanned Cast Interrelation

Figure 5: 15 region details of implant and Scanned Cast Interrelation
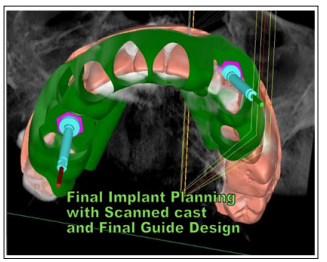
Figure 6: Final DICOM, Cast and Guide design
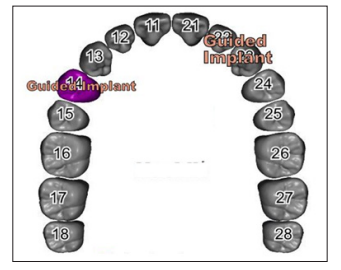
Figure 7: Planned On STL Scanned cast of Patient
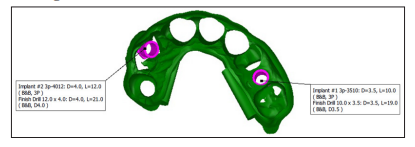
Figure 8: Surgical Protocol
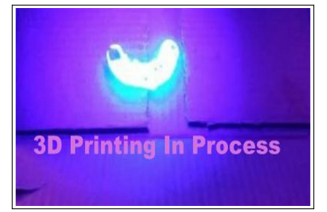
Figure 9: Steriolithotrpic printing of Surgical Guide
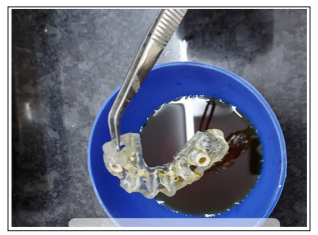
Figure 10: Steriolithotrpic Sterilized Surgical Guide
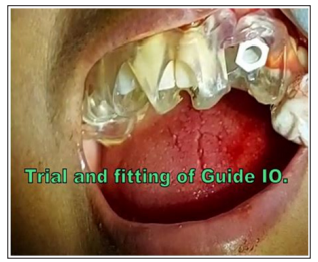
Figure 10: Steriolithotrpic Sterilized Surgical Guide Intraoral Trial

Figure 11: Guided Surgical Kit

Figure 11: Final Implant Placement

Figure 12: Immediate Temporary Prosthesis placement
