Author(s): Yousra Lamarti*, Yassine Smiti, Hniad Adnane, Anas Saoud Tazi
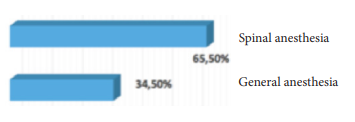
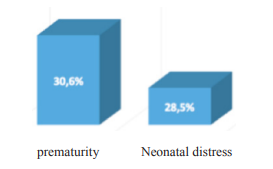
Eclampsia is a very serious complication of pregnancy, its occurrence is responsible of maternal and fetal morbidity and mortality. The aim of this study is to clarify the value of Magnesium Sulfate in the prevention of convulsive state and in the choice of anesthetic technique for cesarean section during eclampsia. We realized a prospective descriptive, analytical and comparative study over a period of 5 months, concerning a series of 49 pregnant women admitted to the anesthesia-intensive care unit of the Souissi Maternity Hospital in Rabat, with eclampsia. The diagnosis of eclampsia was made due to the occurrence of convulsive seizure (s) linked to pregnancy-induced hypertension. It was found that eclampsia mainly affected young women (age less than or equal to 25 years) with a percentage of 57.3%. The majority of patients were first-time mothers (55.1%). This condition manifests itself most often in the last trimester of pregnancy (72.9%), especially in pre-partum. The majority of patients did not receive an antenatal consultation. The treatment of choice in our study was magnesium sulfate. So, 51% of patients had not received magnesium sulfate before their admission to our hospital and 56% of them had had more than one seizure. And the 49% of patients, on the other hand, had received magnesium sulfate and only 18% of them had had the seizure again. Our obstetric attitude was based on immediate delivery with a caesarean section. 34.5% cesarean sections were performed under general anesthesia, compared with 65.5% under spinal anesthesia. The fetus morbidity was mainly represented by prematurity (30.6%) and neonatal distress (28.5%). The prognosis of eclampsia remains bleak both for the mother with a maternal mortality rate of 4%, and for the fetus with a perinatal mortality rate of 16.3%.
Eclampsia is a very serious complication of pregnancy. It is a convulsion associated with high blood pressure during pregnancy. The objective of our study: is to clarify the value of Magnesium Sulfate in the prevention of convulsive attacks and in the choice of anesthetic technique for cesarean section during eclampsia.
This is a prospective descriptive, analytical and comparative study over a period of 5 months concerning a series of 49 parturients admitted to the anesthesia-intensive care unit of the Maternity hospital. Souissi from Rabat, with eclampsia. The diagnosis of eclampsia was made due to the occurrence of convulsive seizure (s) linked to pregnancy hypertension.
Initialy, MgSO4 was used intrathecally, as early as 1906 by Horn to treat the attack of eclampsia. In 1925, Lazard used the intravenous route. The use of MgSO4 has spread in the USA, following the series of Pritchard in 1975 [1]. There has long been a lack of reliable studies to determine the best treatment (anticomitial or MgSO4 ?), Especially because of the small numbers, while the prevalence of eclampsia itself is low, especially in industrialized countries. The first “real”, multi-center international study was published in 1995 and struck a chord with its strong support for MgSO4 [2].
The magnesium (Mg ++) is a predominantly intracellular ion, but its extracellular concentration can modulate the membrane properties of excitable cells (neurons, vascular, cardiac, muscle myocytes). It can block voltage-gated L-type and T-type calcium channels, intracellular calcium channels (sarcoplasm), sodium and potassium channels, ATPase calcium pumps and Na + / Ca ++ transmembrane exchangers.
The imbalance between the extracellular concentrations of Mg ++ and Ca ++ ions, as well as a prolonged calcium entry through L-type channels, would be involved in the genesis of vasospasm; in addition, the vasodilatory effect of MgSO4 is reversed by calcium, while NO antagonists or prostanoids have no effect. The block of calcium channels, by an effect of competition with the Ca ++ ion, therefore seems to be the central point of the vascular effects of MgSO4, especially as the vasodilator effects of MgSO4 are not dependent on the intracellular passage of the ion [3-5].
Magnesium sulfate is a drug of choice for preventing recurrence of an eclampsia attack: it appears to be more effective than benzodiazepines (RR = 0.44; 95% CI: 0.34-0.67), than phenytoin (RR = 0.31; 95% CI: 0.28-0.47) and especially cocktails lytic (RR = 0.09; 95% CI: 0.03-0.24) [6].
Two presentations are theoretically available: sulfate and magnesium chloride. In theory, the chloride would be less toxic [7]. Approximately 10% of women with eclampsia have a second attack of eclampsia on magnesium sulfate. In this case, an additional 2 g bolus of magnesium sulfate may be given over three to five minutes [8].
An inappropriate dosage of Mg is the most common therapeutic error encountered in obstetrics units. Therefore, the patient, throughout this treatment, should have continuous, automated monitoring of heart rate, ECG, blood pressure and SpO2. This instrumental monitoring must be supplemented by the hourly verification of the osteotendinous reflexes, because their disappearance is the first sign of overdose which justifies stopping the infusion.
The antidote is calcium gluconate at a dose of 1g IV [9,10]. Finally, it should be remembered that manifestations of hypocalcemia (spasmophilia) can occur several hours after the interruption of the Mg infusion.
Eclampsia remains a very serious pathology still frequent in our hospital practice, with significant morbidity and mortality both maternal and fetal, especially if the eclampsia is early. These data, far from being satisfactory, may be linked to the rapid and unpredictable evolutionary nature of eclampsia, the lack of awareness among the population, especially in rural areas and the quality of antenatal consultation which is lacking in our context.
Early detection, monitoring of pregnancies, mainly those at high risk, and immediate and adequate medico-obstetrical management improve the maternal-fetal prognosis. Magnesium sulfate, the standard treatment, plays an important role in the prevention of eclampsia. The administration of the latter made it possible in most of our patients to stop the seizure with regained consciousness, which facilitated the choice of locoregional anesthesia (spinal anesthesia) over general anesthesia as a technique for possible extraction.
