Author(s): Kwanhathai Sakulsansern
Background: Intussusception is the most common cause of intestinal obstruction in early childhood. It is an emergent condition where delay in diagnosis leads to an increased risk of bowel perforation and necrosis. Numerous reduction techniques have been described. Safety has to be of prime concern and we strongly believe the air enema technique to be quicker, safer and more effective than liquid enemas. Reduction of intussusception with unsedated child may resist the procedure, which may lengthen its duration and increase the radiation dose. We use intravenous IV sedation during the procedure to overcome these difficulties.
Objectives: The purpose of this study is to determine the effectiveness of our technique for pneumatic reduction under fluoroscopic guidance with IV sedation, using equipment readily available in the hospital, and to study association between the time spent at outside community hospitals prior to transfer and the surgical treatment.
Methods: We retrospectively reviewed cases of pediatric intussusception, from October of 2013 through June of 2020.
Results: A total of 65 patients (35 male, 30 female) with intussusception were treated. Our pneumatic reduction technique was performed in 36 patients, among which 33 (91.67%) cases were successful. No complications occurred. Patients requiring surgery had presented the longer outside community hospital admission length of time.
Conclusion: The technique described is easy to assemble, safe, fast and effective. The surgical morbidity was low in those who were diagnosis early and timely transfer to our center.
Intussusception is the most common cause of intestinal obstruction in early childhood. It is an emergent condition where delay in diagnosis leads to an increased risk of bowel perforation and necrosis [1]. Numerous reduction techniques have been described in many literatures with the advantages and disadvantages of each technique. Pneumatic reduction has a higher success rate and few complications compared to barium enema and hydrostatic reductions. Safety has to be of prime concern and we strongly believe the air enema technique to be quicker, safer and more effective than liquid enemas. Intussusception is related to recent upper respiratory tract infection (URI) which increases respiratory adverse events following general anesthesia for reduction. Reduction of intussusception, may perform on awake children without sedation, but the unsedated child may resist the procedure, which may lengthen its duration and increase the radiation dose. We use intravenous (IV) sedation during the procedure to overcome these difficulties [2, 3]. Intussusception cases usually reported late therefore operative procedure was inevitable and results in significant morbidity and mortality. A study from Ann and Robert H. Lurie Children’s hospital of Chicago showed that a longer time spent at outside community hospitals prior to transfer was associated with higher rates of operative management. This factor may further contribute to difficulty with reduction. By this study we also emphasized on timely transfer to a pediatric surgical center so as to decrease surgical risk [4].
A single center retrospective review was performed at Sawan Pracharak Hospital, which is a pediatric tertiary care hospital in Lower Northern of Thailand. The medical record was queried for all pediatric patients presenting with a diagnosis of intussusception, either as transfer or as primary admission, during the time period from October of 2013 through June of 2020.We retrospectively reviewed cases of intussusception in children aged less than 15 years. Patients were included if they had either abdominal ultrasound (U/S) or computed tomography (CT) evidence of intussusception. Patients were excluded if they did not have radiologic evidence to support the diagnosis of intussusception.
Demographics data were recorded and analyzed including: age, sex, date of admission, symptom with duration, treatment modalities, outcomes, outside community hospital admission length of time (was measured from the time that patient was first admitted to the time that patient arrived at our institution), transfer time (was measured from the time that patient was departed from outside hospital to the time that the patient arrived at our institution), flow processing time (was measured from the recorded admission time to the time at which reduction was perform), procedural time (was measured from the reduction was started to the time which patient was already finished and transferred to ward in a stable conditions) and reduction time.Prior to 2017, all cases of intussusception were managed by barium reduction. From January 2019, the patients were managed by pneumatic reduction.
Statistical analysis patient characteristics data were compared using the Student’s t-test or Mann-Whitney test for continuous variables, and Chi-square or Fisher’s exact test for categorical variables. All statistical analyses were performed with Stata Version14. Statistics were significant with p-value less than 0.05.
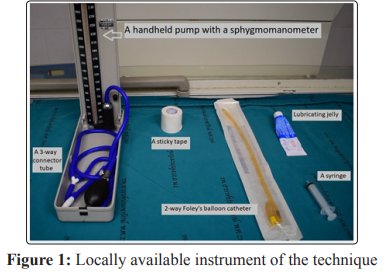
The device used was assembled using equipment readily available
in the hospital (Figure 1)
- A handheld pump with a sphygmomanometer or blood
pressure meter attached to a pressure gauge
- A 20 Fr two-way Foley’s balloon catheter is used to insufflate
the air through the rectum
- A Three-way connector tube
- Lubricating jelly
- An airtight device using a sticky tape
Before attempting the pneumatic reduction, it is ensured that the children were well hydration by venous access and had adequate sedation.
The children were usually frightened and uncooperative. This fear may be exacerbated by pain and parental anxiety. To achieve satisfactory sedation and analgesia, we used intravenous sedation with fentanyl and midazolam before the procedure.
When the intussusception reduced, the children were sent back to the ward.
Initial recording of vital signs was at least every 10 minutes until the child begins to awaken [5].
The safe sedation of children for our procedure requires a clear understanding of the medication’s pharmacokinetic and pharmacodynamic effects and drug interactions (Figure7).
Monitoring include pulse oximetry, heart rate, blood pressure, respiration. Other equipment include suction equipment, adequateoxygen supply, emergency checklist and reversal drugs (Naloxone) [5].

(From U.S. Pharmacist published Adverse Events in Pediatric Sedation, 2008)[5]
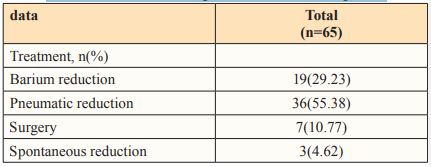
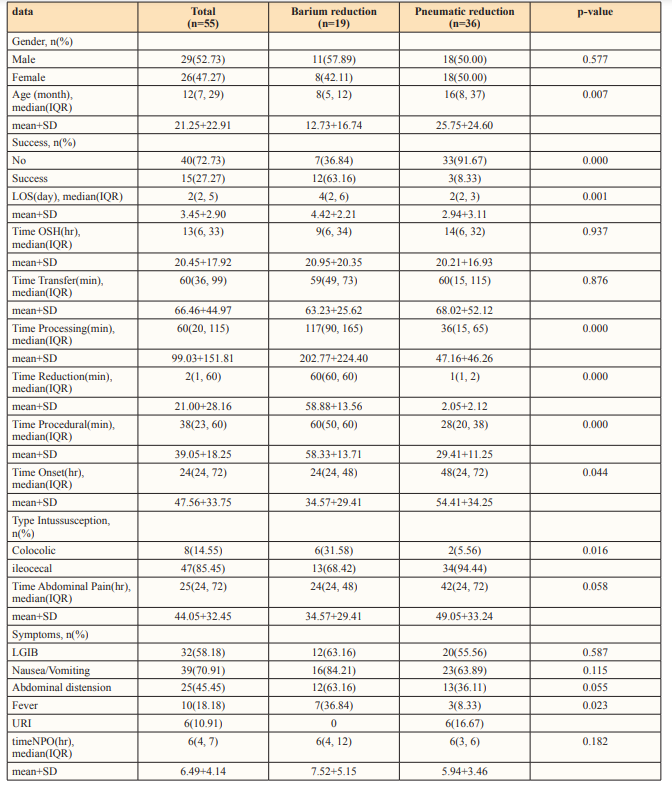
A total of 65 patients (35 male, 30 female) with intussusception were treated at Sawan Pracharak Hospital. The summary of the epidemiological characteristics of all the patients are shown in Table 2 and 3. Seven patients were treated by surgery after the diagnosis due to peritonitis. Three patients had spontaneous reduction after admission in our hospital (Table1).
Mean age at presentation was 23.93+28.90 months (range from 4 to 144 months). Duration of symptoms was 47.72+32.56 hours (range from 7 to 360 hours). The most common symptom reported was abdominal pain, found in all 65 patients. Common present symptoms are represented in Table 3.
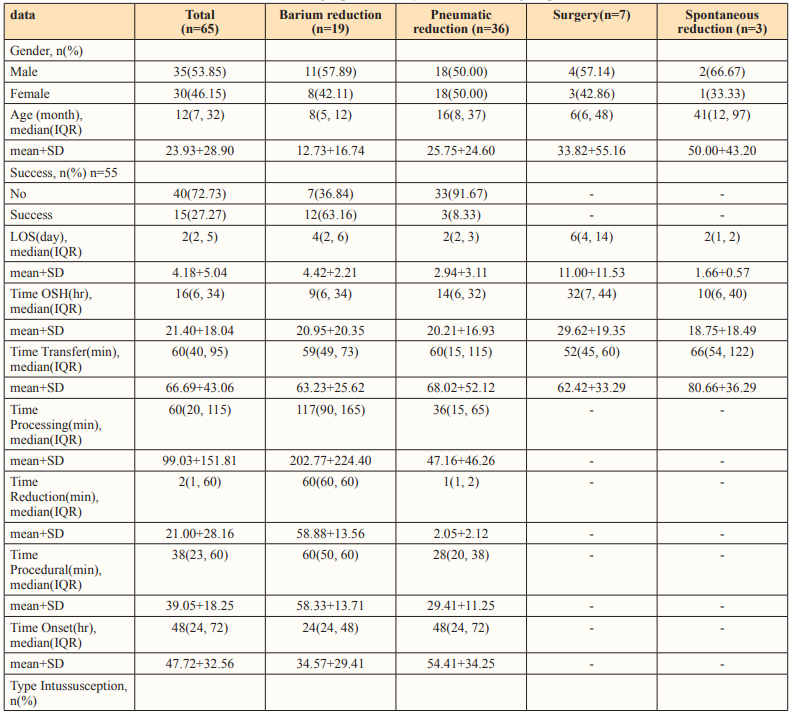
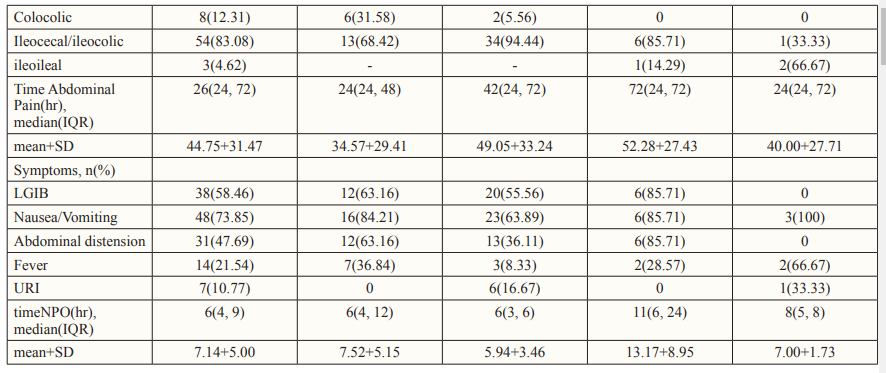
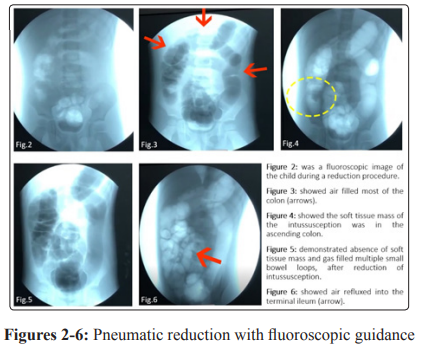
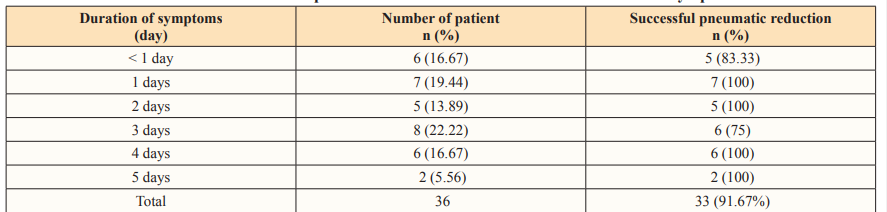
Pneumatic reduction was performed in 36 patients, among which 33 (91.67%) cases were successful, no bowel perforation was observed after procedure. (Table 4 and 6).
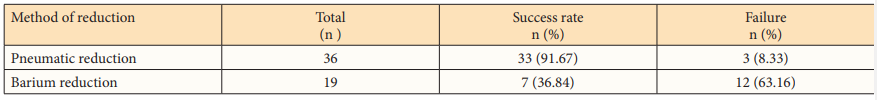
Barium reduction was successful in 36.84% of cases (7 of 19 cases) shown in Table 4. Comparison of pneumatic reduction group and barium reduction group was shown in Table 2. A total of 22 patients in this study (7peritonitis, 15failure of non-operative reduction) required operative treatment. The most frequently performed was laparotomy with manual reduction in unsuccessful barium reduction patients, laparotomy with bowel resection and primary bowel anastomosis in patients with peritonitis and unsuccessful pneumatic reduction. In one case, laparoscopy was made as therapeutic and diagnostic operation after 1st episode of recurrence, but no Meckel diverticulum or other lead point was found.
In our study, 54 (83.03%) patients were ileocolic intussusception, 8 (12.31%) were colocolic type; other types were less common (Table 3). Overall recurrence rate was 4.6% (3 in 65). Early recurrence during same hospitalization in first 24-48 hours was occurred in 2 patients after barium reduction. One patient had a recurrence at three-months follow up after pneumatic reduction (Table 6).
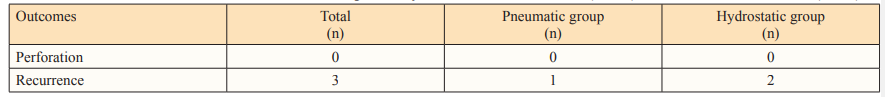
Mean post reduction hospital length of stay (LOS) was 4.18+5.04 days (range from 1-36 days). In pneumatic reduction group mean length of hospital stay was 2.9 days versus 4.4 days in barium reduction group. Mean LOS in surgical group was 11 day. There was a statistically significant difference in length of hospital stay between pneumatic reduction group and barium reduction group (P < 0.05) shown in Table 2. No sedation-related complication was found, including Cardiovascular-related complications (hypotension, hypertension, and cardiac arrhythmias), Respiratory-related complications (respiratory depression, airway obstruction, hypoxia, and pulmonary aspiration), Allergic reactions, or other complications (Nausea and vomiting, paradoxical reactions). IV sedation with Fentanyl and Midazolam did not add any complication to the pneumatic reduction [5].
Regarding time since onset of symptoms, there was a statistically significant difference between pneumatic reduction and barium reduction groups (P < 0.05) (Table 2). The relationship between the longer duration of symptom and the success rate of pneumatic reduction may result in a higher likelihood effectiveness of our safe pneumatic reduction technique than barium hydrostatic reduction methods.
The time required to complete the procedure including procedural time, processing time and reduction time was shorter in the pneumatic group (mean: 29.41+11.25) compare with the barium reduction group (mean: 58.33+13.71). There was no significant difference in transfer time between these two groups (Table 2).
However, we found that patients requiring surgery for intussusception had presented the longer outside community hospital admission length of time (mean: 29.62+19.35 hours) than the successful pneumatic reduction patients (mean: 20.21+16.93 hours) (Table 3).
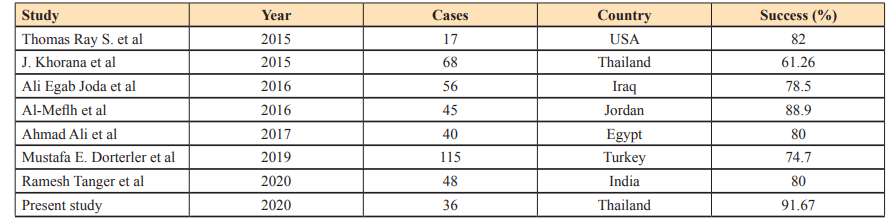
Successful reduction by pneumatic reduction was achieved in 33 patients (91.67%). Recent studies reported rates of successful reduction rage from 61.26% to 88.9% as shown in Table 7.
The higher success rate compared to hydrostatic reduction is due to the inherent compressible effect of air that results in air dissecting between intussusceptum and intussuscipien. Furthermore the well cooperation and the minimal increased intra-abdominal pressure caused by satisfactory sedation resulted in rapid and smooth reduction. We used only minimal to moderate level of sedation, but did not use muscle relaxant or performing general anesthesia because straining during the reduction procedure protects against bowel perforation and decrease risk of respiratory adverse events if the child had previous upper respiratory infection from general anesthesia Apart from higher success rate, our safe technique for pneumatic reduction under fluoroscopic guidance with IV sedation has other advantages. Reduction was faster and therefore the patient received less radiation dose from fluoroscopy. Radiation was further reduced because lower kilo voltage and mill amperage were required. The radiation dose during pneumatic reduction is half that of hydrostatic reduction. Bowel perforation is a known complication in both air and barium reduction. If perforation occurs when barium is used, contamination of the peritoneal cavity with fecal mixed barium is more detrimental than the pneumoperitoneum caused when air is used. When pneumoperitoneum occurs, percutaneous puncture of the abdominal wall with and 18G needle would prevent tension pneumoperitoneum and respiratory embarrassment [7].
Successful management of intussusception imposes early diagnosis, adequate fluid therapy, and early reduction of the invaginating intestinal loops [12]. The long duration of symptoms will give time to development of edema and vascular changes that make the intussusception so tight and decreases the likelihood of pneumatic reduction. In our study, the success rate of pneumatic reduction was 83-100% when the patients presented early in first 24 hours of symptoms and decreased to 75% when the patients present at 72 hours. The same thing was reported by other study, but interestingly, we found that the success rate of our safe pneumatic reduction technique when patients present in 96 -120 hours was 100% (8/8 patients) (Table 5). These may be explained with a reason of using only minimal to moderate level of sedation in our study for well patient cooperation. General anesthesia was not used during pneumatic reduction because it could mask the signs of shock during the procedure. Muscle relaxant was also not used because smooth muscle tension during the reduction procedure protects against bowel perforation. Furthermore the increased intraabdominal pressures caused by straining help rapid reduction [10].
Reduction of intussusception may perform on awake children without sedation, but the unsedated child may resist the procedure, which may lengthen its duration and increase the radiation dose. We use intravenous (IV) sedation during the procedure to overcome these difficulties.
A limitation of pneumatic reduction under fluoroscopic guidance is its limited ability to identify the lead points which cause intussusception during the pneumatic reduction process, and another concern is that fluoroscopic images may fail to depict residual ileoileal intussusception. In our study, under ultrasonographic confirmation after the procedure, we can solve this problem. Furthermore, ultrasonography has high-quality images to detect intra-peritoneal free air [10].
The technique of pneumatic reduction described is easy to assemble, safe, fast and effective. It has high success rate (91.67%) and low complication rate, decrease length of hospital stay. We recommend it for regular use in pneumatic reduction of intussusception. However, the surgical morbidity was low in those who were diagnosis early and timely transfer to our center.
I would like to express my special thanks of gratitude to my teacher “Dr. Nopporn Sritippho” for his valuable guidance and support in completing my research. I would also like to extend my gratitude to “Miss Suraida Aeesoa” for providing me with all the statistical guidance and facility that was required.
