Author(s): Rodrigo Soares de Andrade
The benign migratory glossitis (BMG), for having characteristics of a geographic map is popularly known as the geographic tongue. It is a pathology that affects the dorsum of the tongue, the lesions appear with irregular erythematous plates that have circular shapes with edge bounded by a white-yellowish line, slightly protruding or flat and well-defined, is benign and non-contagious. Its etiology is multifactorial, usually asymptomatic, and may vary fr om size, location, and duration. This work aimed to report an unusual BMG case. A male child, 3 years old, presented a single area of impapilation on the lingual dorsum, after suffering a period of stress, which is repeated every month in exactly the same area. Stress periods can be present at any time in life, and as with adults, can trigger injuries and variations in normality in children. The importance of diagnotic exercise has a direct correlation with the conduct to be taken by the dentist in favor of a good patient prognosis
Benign migratory glossitis (BMG), also described as a geographical tongue, ectopic migratory glossitis, migratory erythema or migratory tongue, is a benign transitional oral condition, which occurs in the regions of the apex, lateral edges and dorsum of the tongue [1-3]. The lesions vary clinically over time and remain from a few hours to several weeks in the mouth [4, 5]. The lesion is characterized by a period of irritation and remission, during which the lesions heal without residual scar development. When lesions return, they tend to appear in new locations and in different shapes, single or multiple, thus producing the migratory effect [7-9].
Its etiology is based on psychological factors (stress), allergic conditions, hormonal disorders, juvenile diabetes, genetic factors, nutritional deficiencies, tongue cracks and hereditary factors [4, 1]. The lesions appear with irregular erythematous plaques that represent the loss of the filiform papillae. They are usually circumscribed, circular, with edges delimited, or at least in part, by a slightly raised yellowish-white or flat and well-defined line [5, 6]. The lesions tend to change location, shape and size within minutes or hours. Any location on the back or lateral edges of the tongue may be affected [10, 11].
Although most patients are asymptomatic, they commonly develop severe anxiety and fear of cancer [1]. The disease is characterized by a period of irritation and remission, during which lesions heal without residual scar development [1-3, 7]. When the lesions return, they tend to appear in new locations, thus producing the migratory effect [2]. In the exacerbation period lesions may be followed by oral discomfort, burning, foreign body sensation, or ear pain [3, 7, 8].
Its diagnosis is made through clinical and historical exams, consistent with chronic, migratory or non-migrant and macroscopic lesions on the epithelium of the tongue that change in size, color and position [5]. Routine laboratory tests, including complete blood count, sedimentation rate. Biopsy and histological examination of the lesions may help in the relief of patients regarding the benign character of the pathology [1].
Histological exams may reveal chronic and acute inflammation infiltrated in the submucosa, with epithelial edema and with neutrophil micro abscesses [7]. The elevated white areas of the lesions contain infiltrated subepithelial neutrophils and micro abscesses, leukocyte invasion in the epithelial layer, interepithelial edema, rupture of the cell junctions, glycogen deposition in the epithelial cells and exfoliation of necrotic cells in the superficial layer [12-14]. Erythematous areas have mononuclear infiltrations in sub and interepithelial positions, two types of basal cells, filament and filament bundle formation in the spiny layer, absence of granular and incomplete keratinized or parakeratinized stratum in the superficial layer [15].
Clinical knowledge of this lesion by the dentist is of great importance, since it is possible to address concerns from patients and family members, especially in the presence of a pediatric patient, and to generate the differential diagnosis of a possible psoriasis. Thus, the objective of this study is to discuss the peculiarities of this condition and to highlight its clinical importance and to highlight an atypical clinical case of unilocular and reicidivant migratory glossitis.
Patient H.D.A, male, was taken by his parents to the dental office for his first appointment with a pediatric dentist at 9 months of age, and no changes were observed. Every four/six months preventive consultations were scheduled for follow-up, also with no relevant changes found. At 3 and a half years of age, the father contacted him reporting that he was very anxious and gnashing his teeth, especially during the day. In the clinical evaluation, wear on the upper and lower incisors was detected, and in the Temporomandibular joint (TMJ) examination no changes were diagnosed.
In conversation with parents for a better understanding of the complaint and the patient’s clinical picture, they reported that 10 months ago the couple’s second child was born and when she completed two months of life she was diagnosed with severe allergy to milk protein, which was demanding much attention and extra care from the parents. After these reports, the hypothesis found was that the stress the child has been going through would have a great connection with wakeful bruxism and consequently overload of the musculature surrounding the TMJ causing the pain, so the patient was referred for psychological evaluation.
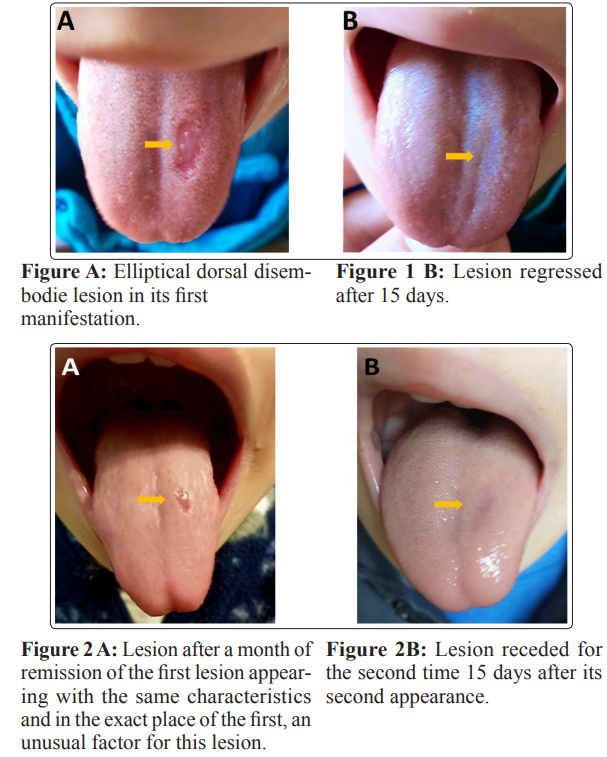
One month after her last visit, the mother contacted her and reported that she was worried about an injury on her son’s tongue that appeared (Figure 1 A), grew and disappeared (Figure 1 B) in a few days, but then appeared again in approximately fifteen days, always with the same characteristics and in the same place (Figure 2 A-B), however the injury did not present painful symptoms. The clinical examination showed a single lesion located on the left dorsum of the tongue, characterized by elliptical reddish erosion, with consequent disappearance of the filiform papillae and preservation of the fungiform papillae, with a defined and whitish border and a little prominent. Due to its clinical and historical aspect, the diagnostic hypothesis was geographical tongue or benign, unilocular migratory glossitis.
Those responsible were advised that there was no need for concern, not even the use of medications to treat this lesion. A new referral for psychological treatment was delivered and requested considering that the lesion was triggered by stress. Orientations to prevent the child from eating acidic, very hot and strong spices were carried out. The child is under further proservation.
The BMG is a benign migratory lesion of the tongue that presents a variable, recurrent and spontaneous healing course. Clinically, it compromises the aesthetics of the tongue and can cause disconfort to the patient such as burning, irritation or sensation of foreign bodies [4-7, 16]. The lesions resulting from this condition may disappear or last for several days, weeks or months of benign but recurrent evolution [4, 5, 16]. The diagnosis is usually clinical and based on the characteristic history of migration, the characteristics of the lesion, the circled aspect and the lack or presence of significant pain as opposed to burning as a subjective complaint [11, 16].
In the presented case, the patient presented only a variable course, recurrent and spontaneous healing lesion, but distinct from the literature when the lesions commit several parts of the dorsum and lateral tongue, and in the case presented its recurrence always affects the same place. The diagnosis was made only with clinical examination, based on the characteristics of the lesion, absence of migration and significant pain, and the report of periods of stress suffered by the child.
Related to the development of the lesion are conditions: genetic, hereditary, psoriasis, hormonal disorders, emotional stress or consumption of acidic, hot or spicy food and tongue fissure commonly associated with heredity and uncommon in children, which is distinct in the case presented, as a child presented this variation of normality after critical periods of stress [4, 5, 8, 9,16, 12, 13].
Some studies affirm in their study under predilection of the lesion by the female gender of 5:3 and 2:1, respectively, different from the case presented, that it is a boy [17-19]. In the case presented, there was disagreement regarding the age and health condition of the study subject. However, the literature correlates the presence of BMG more frequently in the presence of allergies or hereditary factors and also to the emotional factor, suggesting drug treatment only in symptomatic cases and orientation in asymptomatic cases,
Commonly, BMG can be associated with psoriasis because it is an oral manifestation that occurs more frequently in these cases and because of the similarity of clinical presentation, histology and immunohistochemical findings, being related with a lesion [20, 21]. However, the health condition of the study individual is highlighted. Regarding treatment, the literature points out that drug treatment can be performed in cases of intense symptoms. However, in cases of absence of symptoms, there is no need, using only oral hygiene instructions [2, 3, 20]. In this case, only oral hygiene instruction and motivation, referral to a psychologist, and periodic follow-up were necessary.
Stress periods can be present at any time in life, and as with adults, can trigger injuries and variations in normality in children. The dentist’s knowledge of variations in normality and their causes has a direct influence on the physical and psychological aspect of the patient, since their manifestations have a multifactorial origin, so knowing how to diagnose and treat when necessary has a direct correlation with a good prognosis.
The National Council for Scientific and Technological Development - CNPq, Brazil
None declared.
The dissemination of images and information on the identification of the patient by the responsible persons was authorized.
1.Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M (2002) Benign Migratory Glossitis or Geographic Tongue: An Enigmatic Oral Lesion, The American Journal of Medicine 113:751-755.
2.Zargari O (2006) The prevalence and significance of fissured tongue and geographical tongue in psoriatic patients. Clin Exp Dermatol 31: 192-5.
3.Menni S, Boccardi D, Crosti C (2004) Painful geographic tongue (benign migratory glossitis) in a child. European Academy of Dermatology and Venereology, JEADV 18: 736-748.
4.Desai VD, Phore S, Baghla P (2015) Asymptomatic reversible lesion on tongue – case series in pediatric patients. Arch Med Health Sci 3: 113-116.
5.Abe M, Sogabe Y, Syuto T, Ishibuchi H, Yokoyama Y, et al. (2007) Successful treatment with cyclosporin administration for persistent benign migratory glossitis. J Dermatol 34: 340-3.
6.Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M (2002) Benign migratory glossitis or geographic tongue: an enigmatic oral lesion. Am J Med 113: 751-5.
7.Masferrer E, Jucgla A (2009) Geographic tongue. N Engl J Med 361: 44.
8.Jainkittivong A, Langlais RP (2005) Geographic Tongue: Clinical Characteristics of 188 Cases. JCDP 6: 123-35.
9.Rioboo-Crespo Mdel R, Planells-del Pozo P, Rioboo-Garcia R (2005) Epidemiology of the most common oral mucosal diseases in children. Med Oral Patol Oral Cir Bucal 10: 376- 87.
10.Hooda A, Rathee M, Gulia J,Yadav S (2011) Benign migratory glossitis: a review. Internet J Fam Pract 9: 1-7.
11.Nandini DB, Bhavana SB, Deepak BS, Ashwini R (2016) Paediatric geographic tongue: a case report, review and recent updates. J Clin Diagn Res 10: 5-9.
12.Assimakopoulos D, Patrikakos J, Fotika C, Elisaf M (2002) Benign Migratory Glossitis or Geographic Tongue: An Enigmatic Oral Lesion. Am J Med 113: 751-755.
13.Menni S, Boccardi D, Crosti C (2004) Painful geographic tongue (benign migratory glossitis) in a child. JEADV 18: 737-738.
14.Shekhar MG (2014) Geographic Tongue in Monozygotic Twins. J Clin Diagn Res 8: 1-2.
15.Miloglu O, Goregen M, Akgul HM, Acemoglu H (2009) The prevalence and risk factors associated with benign migratory glossitis lesions in 7619 Turkish dental outpatients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod; 107: 29-33.
16.Picciani BLS, Domingos TA, Teixeira-Souza T, Santos VCB, Gonzaga HFS, et al. (2016) Geographic tongue and psoriasis: clinical, histopathological, immunohistochemical and genetic correlation – a literature review. An Bras Dermatol; 9: 410- 421.
17.Picciani B, Santos VC, Teixeira-Souza T, Izahias LV, Curty A, et al. (2017) Ivestigation of the clinical features of geographic tongue: unveiling its relationship with oral psoriasis. Int J Dermatol 56: 421-427.
18.Banoczy J, Szabo L, Csiba A (1975) Migratory glossitis. A clinical-histologic review of seventy cases. Oral Surg Oral Med Oral Pathol; 39: 113-21.
19.Menni S, Boccardi D, Crosti C (2004) Painful geographic tongue (benign migratory glossitis) in a child. J Eur Acad Dermatol Venereol 18: 737-8.
20.Masferrer E, Jucgla A (2009) Images in clinical medicine. Geographic tongue. N Engl J Med 361: 44.
21.Rioboo-Crespo Mdel R, Planells-del Pozo P, Rioboo-Garcia R (2005) Epidemiology of the most common oral mucosal 376-87.
View PDF