Author(s): Chin Hong Ngai*, Angela Bin Bin Zhan, Sophie Jia Qian Koh, Audrey Jia Luan Tan and Vincent Diong Weng Nga
ABSTRACT
Background: The pituitary gland is prone to various lesions, and the endoscopic transsphenoidal approach is a minimally invasive surgical technique
for removing such lesions. Surgical removal of part or all pituitary lesions can result in an empty sella turcica, potentially causing herniation of the optic chiasm. This report presents three cases of patients who developed visual impairment following pituitary surgery and were diagnosed with herniation of the optic chiasm into an empty sella turcica.
Case Series: We report three cases of visual deterioration following transsphenoidal resection, with MRI findings indicating optic chiasm herniation. These cases underscore the complexity of post-surgical outcomes and the potential mechanical impact on the optic chiasm.
Case 1: A 65-year-old man underwent surgery for a Rathke’s cleft cyst, resulting in initial unchanged vision, followed by worsening bitemporal hemianopia despite successful cyst removal. Post-operative imaging suggested optic chiasm herniation, with subsequent hormonal disturbances developing 4 weeks after surgery.
Case 2: A 62-year-old man with a history of macroprolactinoma, initially treated with dopamine agonists, experienced progressive vision loss despite medical therapy, leading to surgical intervention. Post-surgery, prolactin levels improved, but visual acuity continued to decline, with imaging showing persistent optic chiasm herniation 6 weeks post-operation.
Case 3: A 37-year-old man, previously treated for a pituitary adenoma via transsphenoidal surgery, presented with worsening bitemporal hemianopia 96 weeks post-surgery. MRI revealed downward traction of the optic chiasm, suggesting long-term mechanical effects impacting vision.
Conclusion: This case series highlights that patients presenting with visual changes and a history of recent pituitary gland surgery should be investigated for herniation of the optic chiasm into the sella turcica.
The pituitary gland is a small yet crucial endocrine organ at the brain’s base that regulates various hormonal functions [1]. Pituitary lesions, including adenomas, craniopharyngiomas, Rathke’s cleft cysts, and rare carcinomas, manifest through hormonal imbalances, headaches, and vision problems, depending on their type, size, and hormone secretion [2]. Transsphenoidal resection, a minimally invasive surgical technique, is preferred for removing pituitary tumors not extensively spread beyond the gland due to its quicker recovery, reduced discomfort, and fewer complications compared to craniotomy [3]. However, risks include infection, bleeding, damage to optic nerves or the brain, cerebrospinal fluid leaks, and hormonal imbalances [4].
While the primary goal of transsphenoidal surgery is to alleviate pressure on the optic nerves or chiasm, vision loss remains a potential complication [5]. Causes include direct trauma, vascular compromise, inflammation, infection, and postoperative hematoma [4]. Prompt evaluation and management, often requiring further imaging or intervention, are essential.
Optic chiasm herniation, particularly following treatments for pituitary disorders like prolactinomas treated with dopamine agonists, has been increasingly recognized [6]. Rapid tumor shrinkage can lead to chiasmal prolapse, confirmed through magnetic resonance imaging (MRI) [6]. However, herniation of the suprasellar visual system after transsphenoidal surgery is rarely reported. This report presents three cases of visual impairment post-pituitary surgery, diagnosed with optic chiasm herniation into an empty sella turcica.
A 65-year-old man with no prior medical issues presented with bitemporal hemianopia, frequently colliding with objects. He was initially seen in an Ophthalmology clinic on 6/10/2020 and referred to Neurosurgery on 13/10/2020. Pre-operative hormonal analysis on 20/10/2020 revealed normal renal function and hormone levels, including adrenocorticotropic hormone (ACTH), cortisol, growth hormone, insulin-like growth factor 1 (IGF-1), thyroid function, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and prolactin. A visual assessment confirmed complete bitemporal hemianopia and color vision impairment, with no anisocoria or relative afferent pupillary defect (RAPD). MRI on 12/10/2020 identified a large, lobulated, non-enhancing sellar-suprasellar lesion (3.2 x 4.6 x 2.4 cm), hypo-intense on T1WI and hyper- intense on T2WI, suggestive of a Rathke cleft cyst.
The patient underwent endoscopic endonasal transsphenoidal fenestration on 26/10/2020, confirming the Rathke cleft cyst and resulting in a small intraoperative cerebrospinal fluid (CSF) leak. Post-operative histology was consistent with the cyst. Post- operatively, the patient reported unchanged vision. Post-operative ophthalmology review showed some improvement but persistent bitemporal hemianopia.
Subsequent 1-month post-surgery appointments revealed ongoing vision problems, with overlapping words and missing letters, and worsening bitemporal hemianopia. Post-operative hormonal profiles indicated decreased cortisol levels and hormonal imbalances, including central hypothyroidism, hypocortisolism, and central diabetes insipidus. Follow-up MRI showed no remnant cystic lesion but thinning and slight herniation of the optic chiasm, as shown in Figure 1. As of the last review on 6/10/2022, the patient continued to suffer from panhypopituitarism and poor vision.
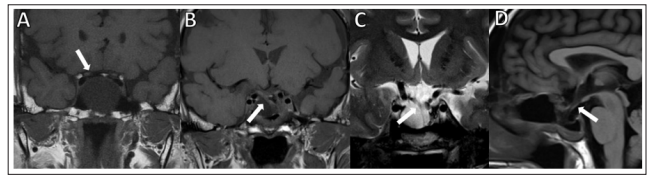
Figure 1: MRI of the pituitary showed upward bowing of optic chiasm caused by compression of Rathke Cleft cyst preoperatively, and MRI of the pituitary showed optic chiasm herniation after surgery
A 62-year-old male with a history of hyperlipidemia and osteoporosis presented to the Ophthalmology Clinic in November 2014 with gradually worsening left visual blurring over several months. Humphrey Visual Field (HVF) assessment revealed bitemporal hemianopia. MRI on 19/12/2014 identified a lobulated enhancing mass (2.4 x 2 x 2 cm) in the sellar region, extending suprasellarly towards the hypothalamus, compressing the optic chiasm, and beginning to encase the left cavernous sinus. The patient reported progressive left-sided visual blurring. Endocrine tests in early December 2014 showed significantly elevated prolactin levels >10000 mIU/L (reference range: 86-324). The diagnosis was macroprolactinoma, leading to hypogonadotropic hypogonadism and central hypothyroidism. Treatment with cabergoline (0.5 mg twice weekly) and levothyroxine (25 mg) was initiated.
Initially responding well, the patient defaulted from treatment between June 2017 and November 2019. The resumption of cabergoline in December 2019 failed to produce a biochemical response, and the tumor size increased. Despite increasing cabergoline to 6 mg/week by April 2022, the tumor growth remained uncontrolled, indicating probable secondary resistance. Surgical intervention was necessitated. After initially refusing, the patient finally consented to endonasal transsphenoidal resection of the macroprolactinoma, performed successfully on 14/9/2022 without CSF leakage, improving vision perception post-operatively. Post- surgery, prolactin levels were significantly reduced, and histology confirmed a pure lactotroph pituitary adenoma.
However, an ophthalmological review on 28/10/2022 showed worsening blurred vision in the left eye, noticeable when reading. Examination revealed that the left eye showed grade 2 RAPD, impaired color vision, temporal hemianopia in the right eye, and generalized depression in the left eye on HVF testing. Post- operative visual acuity had declined compared to pre-operative levels. Subsequent MRI demonstrated herniation of the optic chiasm, as shown in Figure 2. Unfortunately, the patient’s vision showed no improvement upon the latest evaluation.

Figure 2: T1-weighted MRI of the pituitary axial view, arrow showed herniation of optic chiasm after surgery
In 1996, a 37-year-old man was diagnosed with panhypopituitarism, necessitating hydrocortisone and thyroxine replacement therapy. MRI revealed features of a pituitary adenoma, and he underwent a transsphenoidal resection the same year. In 2013, the adenoma recurred, requiring a second transsphenoidal resection, which histopathology confirmed as a pituitary adenoma.
In June 2016, the patient experienced worsening bitemporal hemianopia. MRI revealed inferior herniation of the optic chiasm,as shown in Figure 3. Since then, both his MRI changes and vision have remained stable without notable worsening in 2024.

Figure 3: MRI of the pituitary showed upward bowing of optic chiasm caused by compression of pituitary adenoma preoperatively, and MRI of the pituitary showed optic chiasm herniation after surgery
Table 1: Describes Each Case with Unique Aspects of Patient History, Type of Pituitary Lesion, Visual Improvement, Complications, and Outcomes, Particularly Regarding Visual Changes. for Case 3, There Is No Documentation on Post-Operative Visual Symptoms

From the three cases, a common pattern emerged where there was initial improvement in visual symptoms post-surgery, followed by subsequent deterioration. Optic chiasm herniation and associated visual changes can also manifest after a considerable delay post-surgery, as seen in Case 3. Unfortunately, none of the patients showed improvement after the diagnosis of optic chiasm herniation. Therefore, patients presenting with visual changes and a history of recent pituitary gland surgery should be evaluated for optic chiasm herniation into the sella turcica. These findings underscore the importance of informing patients about the potential for worsening visual symptoms post-surgery and the possibility of permanent deficits despite the low likelihood of occurrence.
Vision deterioration following surgical interventions, though relatively infrequent with an incidence as low as 0.6% for transsphenoidal surgery, carries significant clinical implications [7]. The current literature inadequately covers vision loss after pituitary lesion surgery and existing predictive models fail to anticipate this outcome effectively. In a significant study by Rutland et al. in 2022, 587 patients were analyzed for vision loss post-surgery. This included 11 patients who noted a decline in their vision and three who experienced vision loss after undergoing an endoscopic procedure [8]. There is a noticeable gap in research specifically addressing patients who experience worsening vision following endoscopic surgery on the pituitary gland.
Visual deterioration can be multifactorial, encompassing mechanical displacement and vascular compromise. Under normal conditions, the optic chiasm is shielded from mechanical stress by its anatomical position within the suprasellar cistern, protected by the diaphragma sellae [9]. However, surgical alterations or defects such as a compromised diaphragma sellae can predispose the optic chiasm to herniate into the sella turcica, potentially causing visual loss [10]. Interestingly, the degree of herniation does not always correlate directly with visual impairment severity, suggesting additional factors like vascular insufficiency or neurotoxicity may play significant roles [11]. Delayed visual loss and optic chiasm herniation have been reported following dopamine agonist treatment for prolactinomas due to rapid tumor shrinkage causing chiasmal prolapse [6]. Despite effective tumor reduction, recurrent visual loss due to chiasmal herniation can occur without tumor recurrence. This underscores the dynamic changes within the sellar region impacting the optic chiasm post-treatment. The absence of tumor regrowth and continued visual deterioration imply that mechanical factors alone may not fully explain the observed visual changes, with potential contributions from drug toxicity or ischemic processes due to vasospasm [12].
The advancement in surgical techniques and imaging has made optic chiasm herniation an emerging concern in the postoperative management of transsphenoidal pituitary surgery patients. Our case series and literature review highlight the multifactorial nature of postoperative visual deterioration, where mechanical displacement and vascular compromise are significant factors. The patient in case 1 continued to suffer from visual and hormonal problems after a transsphenoidal surgery to excise a Rathke cleft cyst. Despite MRI evidence of optic chiasmal herniation indicating ongoing mechanical effects on the optic chiasm, it is crucial to consider vascular disturbances as a contributing factor. The range of outcomes—from initial improvement to a gradual decline in visual sharpness—underscores the complex and diverse nature of postoperative visual deterioration. This case illustrates that mechanical traction from optic chiasm herniation may not be the sole cause of visual issues, pointing to a possible significant role for vascular compromise in the patient’s persistent visual and hormonal difficulties.
Current literature lacks long-term follow-up data regarding optic chiasm herniation. In case 3, this patient was diagnosed with optic chiasm herniation with visual deterioration in 2016. In 2024, the optic chiasm herniation did not regress, and the patient remained visually impaired. Thankfully, there has been no further deterioration of vision since 2016, yet there has been no improvement.
Chiasmopexy, a surgical intervention for symptomatic chiasmal herniation, aims to reverse visual field losses by alleviating mechanical stress on the optic chiasm [13]. Various approaches, such as transcranial, transsphenoidal, and transglabellar, have advantages and challenges [13]. Using different materials for sellar packing, from autologous tissues like fat and bone to synthetic materials like silicone, adds complexity to patient management decisions [14]. Ishihara et al. (2018) recommended less absorbable autologous materials to minimize infection risks. Intraoperative MRI can optimize sellar packing, ensuring adequate but not excessive packing and potentially improving outcomes [14]. However, chiasmopexy carries surgical risks, including CSF leaks, infections, and bleeding, particularly in patients with previous transnasal transsphenoidal surgeries. These risks are heightened if the patient has previously had transnasal transsphenoidal surgery and opts for the transsphenoidal approach once more [15]. While chiasmopexy has been employed to address secondary visual field loss due to chiasmal herniation, its effectiveness remains debatable. Despite the mechanical relief provided by chiasmopexy, the controversy surrounding the efficacy of this procedure is noteworthy, as not all patients experienced an improvement in visual outcomes [10]. Complicated and unclear pathophysiological mechanisms, including traction, vascular compression, or kinking of the chiasm, complicate decision-making. Adherence of the chiasm to the diaphragm sellae during initial transsphenoidal surgery may compromise vascular supply and contribute to visual deterioration, making subsequent chiasmopexy decisions particularly challenging due to uncertain outcomes. The decision to pursue chiasmopexy should be considered carefully, weighing the specific clinical scenario, symptoms, and potential risks and benefits, particularly given the uncertain outcomes associated with chiasmopexy.
In this case series, different neurosurgeons offered chiasmopexy to patients at different timelines. Still, given the uncertainty in treatment efficacy and risks of surgery, all of them have declined surgery. Our findings, aligned with current literature, suggest that while optic chiasm herniation is a plausible mechanism for visual impairment post-transsphenoidal surgery, the decision for chiasmopexy should be carefully considered.
One significant limitation of our study is its retrospective nature. This design inherently restricts access to prospective data collection and may limit the depth and breadth of information available for analysis. Data were collected from records, and detailed information might not be accessible due to the transition to digital record-keeping. This can lead to inconsistencies in data quality and availability, potentially affecting the robustness and generalizability of our findings. For example, specific details about the timing of symptom onset or the exact nature of postoperative care might not be consistently recorded, which can obscure subtle but critical influences on patient outcomes, particularly evident in Case 3. Fortunately, the MRI images for this case were well- preserved and of high quality, providing a reliable reference point for analysis.
While our case series provides valuable insights into the complexities of optic chiasm herniation and its impact on visual outcomes, the relatively small number of cases may limit the generalizability of our findings. With a larger sample size, more robust statistical analyses could be performed, enhancing the understanding of various factors influencing the success of surgical interventions and visual outcomes. Additionally, a more extensive dataset might allow for identifying the sole effect of mechanical traction in optic chiasm herniation without another confounding mechanism, such as vascular compromise, that could inform treatment strategies and predictive assessments.
Our review of clinical case studies underscores the need for vigilant monitoring and individualized management of optic chiasm herniation after transsphenoidal surgery. This condition requires enhanced surgical precision, improved predictive models for visual outcomes, and a multidisciplinary approach to post-pituitary surgery care. Patients with visual changes post-pituitary surgery should be evaluated for optic chiasm herniation, as deterioration can follow initial improvement. It is crucial to inform patients about the potential for worsening visual symptoms and possible permanent deficits.
Nil
